Recent confirmation of Zika outbreaks in Pakistan underscores the virus’s potential for undetected spread — with global public health implications.
Last week, researchers solved a longstanding infectious disease mystery. But rather than putting matters to rest, their discovery has precipitated broader public health implications — both in Pakistan and beyond.
Since 2021, BlueDot has been closely monitoring annual reports from Pakistan of outbreaks of an “unknown febrile-like illness” in Karachi. Last week, the results of a retrospective study confirmed that the unspecified disease was Zika — officially documenting the first-ever Zika outbreak in Pakistan.
Given those findings, the virus that went undetected is anticipated to cause recurring outbreaks. But limited laboratory and surveillance capacities in Pakistan and other countries, including a lack of disease reporting systems, render the virus’s magnitude and impact poorly understood. That’s especially concerning with Zika, which is known to evade detection due to its typically mild dengue-like symptoms and its distinctive transmission pathways among arboviruses — yet whose later complications can have devastating effects.
“The concern with emerging pathogens is that we may not know all of the clinical implications until likely many years later,” says BlueDot’s head of surveillance Dr. Mariana Torres Portillo. During the 2015-2016 Zika outbreak in Brazil, it wasn’t until a strange uptick in neurological syndromes was noticed, months into the outbreak, that the virus’s serious complications became known. Important among them are microcephaly and other genetic malformations in babies whose mothers become infected with Zika virus while pregnant, as well as Guillain–Barré syndrome among adults. As it flies under the radar, Zika virus poses substantial public health risks for both endemic and non-endemic regions where the vector is present.
Zika: Behind the arbovirus
Zika virus is a mosquito-borne illness first identified in humans in Africa in the early 1950s. The primary culprit for transmission is the Aedes aegypti mosquito – the same insect that can spread dengue, chikungunya, and yellow fever. But perhaps unique among arboviruses (that is, infections resulting from the bite of an infected insect), Zika can also be sexually transmitted.
Since its discovery, Zika has emerged in countries across tropical and subtropical regions. In 2007, the first large human outbreak occurred on Yap Island in Micronesia, affecting almost three quarters of the population. Six years later, Zika virus spread from this small island east of the Philippines to other Pacific islands, including French Polynesia, Easter Island, the Cook Islands, and New Caledonia. In early 2015, the virus arrived in South America, causing large outbreaks in Brazil and Colombia before being declared a Public Health Emergency of International Concern. By the end of 2016, approximately 175,000 cases had been confirmed across the Americas, with several hundred thousand more suspected. And in 2019, locally acquired cases of Zika virus were reported in France, calling into question the possibility of further spread across Europe.
As of May 15, 2024, Zika virus has emerged in around 90 countries globally (see image); Pakistan can now be included in that list. However, it is possible that other countries without strong surveillance capacities have undetected Zika virus outbreaks — and many could still be at risk
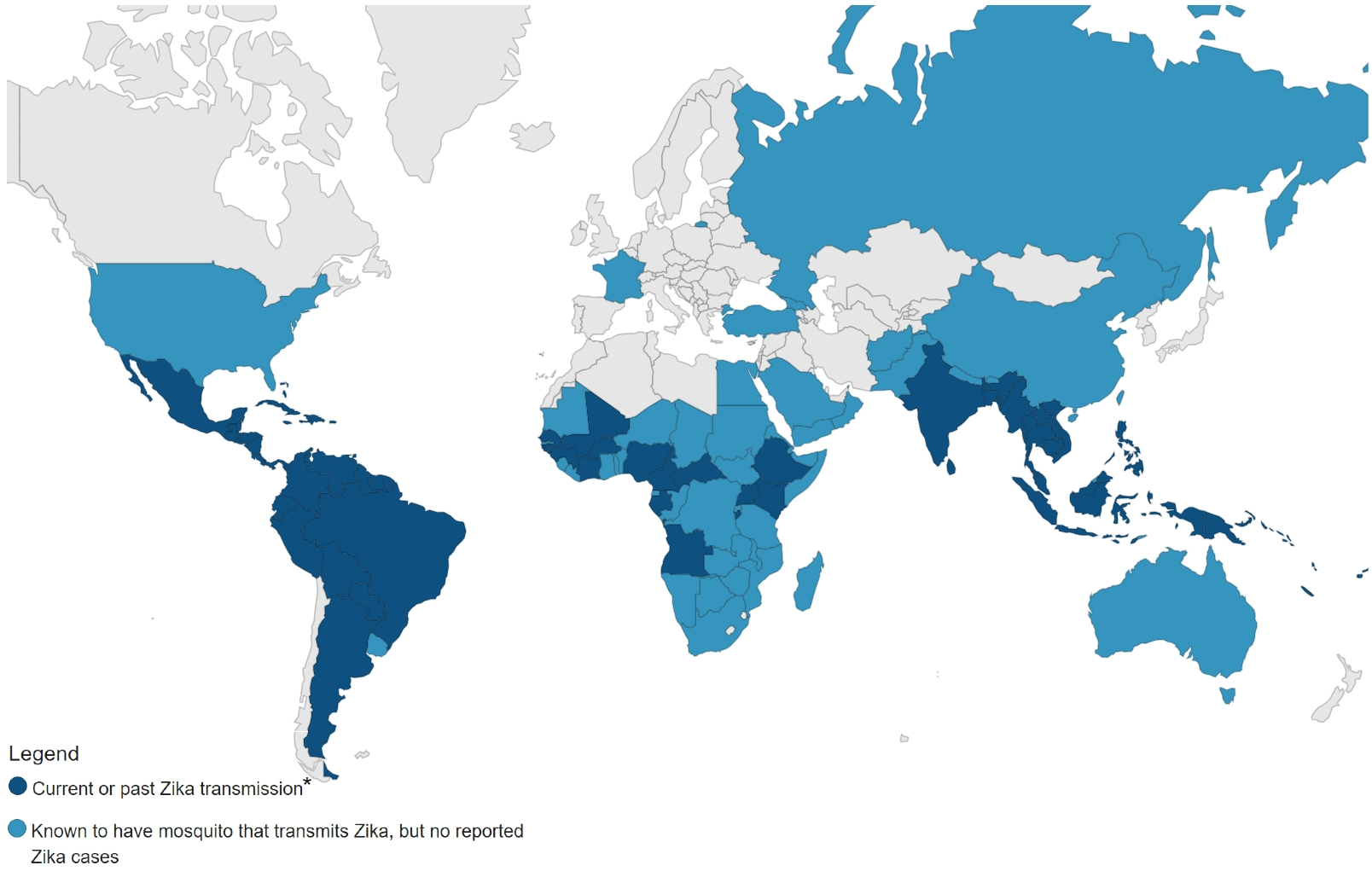
*Known activity over the previous 12 months for temperate countries with strong surveillance systems, and any historical activity for tropical countries. Source: CDC
Zika virus infection is often asymptomatic, with only a quarter of those infected developing symptoms. Any symptoms that do emerge are usually mild and nonspecific, like low-grade fever, rash, and headache, and they resolve within a week — all of which can result in outbreaks being initially undetected. Rarely, but consistently, Zika infection results in profound neurological effects. Around 5% of newborns whose mothers were infected while pregnant have Zika-associated birth defects, including microcephaly – a condition marked by a smaller head size and brain that can lead to neurodevelopment disabilities. Notably, the risk of congenital anomalies is increased if infection occurs in the first trimester.
Adults who contract Zika may develop Guillain–Barré syndrome, a rare autoimmune disorder in which the immune system attacks the peripheral nervous system, causing weakness and, in severe cases, paralysis and difficulty breathing. To date, there is no treatment, prophylactic drug, or vaccine for Zika virus.
Zika: 3 Top Takeaways
1. Zika is flying under the radar but may be the underlying cause of an initially unknown febrile illness. Uncovering the first historical confirmation of a Zika virus outbreak in Pakistan, retrospective data show how Zika has gone undetected because of limited laboratory and surveillance capacities.
2. Zika presents diagnostic difficulties and devastating effects. With similar symptoms to dengue and other arboviruses, clinical diagnosis of Zika is challenging, and its mild clinical presentation is often overlooked. Yet, it poses serious neurological complications, including infant microcephaly and Guillain-Barré syndrome.
3. Strengthening surveillance systems is critical. Amid a lack of vaccines or treatments, improved monitoring is needed, especially in nations with fewer resources. With this, Zika virus can be more effectively tracked and diagnosed in those who have been infected, and necessary public health interventions, such as mosquito control measures and travel advisories, can be initiated.
Public health implications and preventative measures
Official Zika case counts worldwide are down since their 2016-17 peak and have not risen dramatically since. But the situation in Pakistan underlines how Zika is particularly prone to being under-reported, which is concerning given its substantial public health risks. Severe illness has long-term effects on patients, including congenital abnormalities, severe disability, and early death. That’s why we are seeing France take extra measures to mitigate infectious disease outbreaks, including Zika and other mosquito-borne illnesses, ahead of the 2024 Paris Olympics beginning later in July. Moreover, Zika outbreaks can substantially impact families of children born with congenital Zika syndrome, some of whom require continuing and specialized care.
With no available treatments or vaccinations, surveillance to identify outbreaks is the most important element in Zika detection and prevention. Bolstering disease monitoring efforts is crucial, especially for local populations. Public health officials should educate front-line clinicians about Zika to ensure it is considered in differential diagnoses for certain presenting symptoms and negative test results. Accurate, up-to-date understanding of Zika virus activity can be used to update travel advisories which can ultimately protect the most at-risk groups: those who are or are planning to become pregnant.
Individuals can also adopt several preventative measures to minimize transmission of communicable diseases such as Zika and dengue. For one, people should consider avoiding travel to areas where outbreaks are occurring, especially if they are at risk. If travel to an affected region is necessary, bug spray, long-sleeved clothing, and mosquito nets should be used. Additionally, abstaining or using barrier-method contraception is the best way to mitigate sexual transmission. And since the virus can remain in bodily fluids for several weeks, these protective measures should be continued for up to three months after travel to an affected region or when symptoms first emerge. Finally, though vaccine candidates are in early phases of development, immunization against Zika may become an essential step in controlling disease spread.
BlueDot, whose surveillance and modeling systems correctly predicted the international spread of Zika during the 2015 outbreak in Brazil, remains at the forefront of tracking emerging pathogens around the globe. By combining AI and a dedicated surveillance team, BlueDot provides updates, alerts, and critical public health information for Zika virus and beyond. To keep updated, sign up here to receive every edition of BlueDot Outbreak Insider.









