Declining vaccination rates and expansion to non-endemic regions leave many at risk of disease from this severe mosquito-borne virus
On March 26, 2025, the Pan American Health Organization/World Health Organization (PAHO/WHO) released a joint epidemiological alert for yellow fever in the Americas. In the first three months of 2025, 131 confirmed cases and 53 deaths have been reported — already doubling cases from all of 2024. And because yellow fever often goes underdetected due to its clinical similarities to other vector-borne diseases such as dengue and malaria, true case counts are suspected to be as much as ten times higher.
Brazil, Colombia, Peru, and Bolivia are the nations currently reporting cases. Although yellow fever is endemic to Amazonian parts of these countries, the virus has emerged in previously unaffected areas, including São Paulo, Brazil, and Tolima, Colombia. “The worry is less about a pandemic emerging and more about the virus spreading to areas with high proportions of vulnerable people,” says Dr. Mariana Torres Portillo, BlueDot’s head of surveillance.
The majority of cases are among those who are unvaccinated as the region experiences declining vaccination rates. Between 2014 and 2023, approximately half of the countries with endemic areas experienced a decline in vaccination, especially during the peak years of the COVID-19 pandemic. In 2023, the endemic region of the Americas only had 63% coverage, resulting in a large susceptible population.
As PAHO calls on member states to boost public health measures amid spiking yellow fever cases, this edition of Outbreak Insider will delve into this lesser-known mosquito-borne infectious disease.
Yellow fever’s storied history and urban adaptation
Yellow fever, named for the jaundiced appearance that occurs in severe stages of infection, is an acute hemorrhagic disease transmitted by the same mosquitoes that carry more well-known arboviruses such as dengue, chikungunya, and Zika.
Its origins go back thousands of years to the rainforests of Africa. First circulating between mosquitoes and non-human primates, the virus adapted to infect humans during a natural climate change event, when the Sahara was transforming from grassland to desert. By the 17th century, the disease had emerged in the Americas during the transatlantic slave trade as mosquitoes bred in water barrels on board and infected the enslaved. Mosquitoes then spread onto land, leaving major yellow fever epidemics in their wake.
Today, the virus is primarily localized to Africa and the Americas, where the climate provides conducive habitat for the vector species. Three transmission cycles have been identified: sylvatic (jungle), intermediate (savannah), and urban. The sylvatic cycle is what typically drives outbreaks in the Americas, while the intermediate cycle is exclusive to Africa.
Yellow Fever Transmission Cycle in (A) South America and (B) Africa
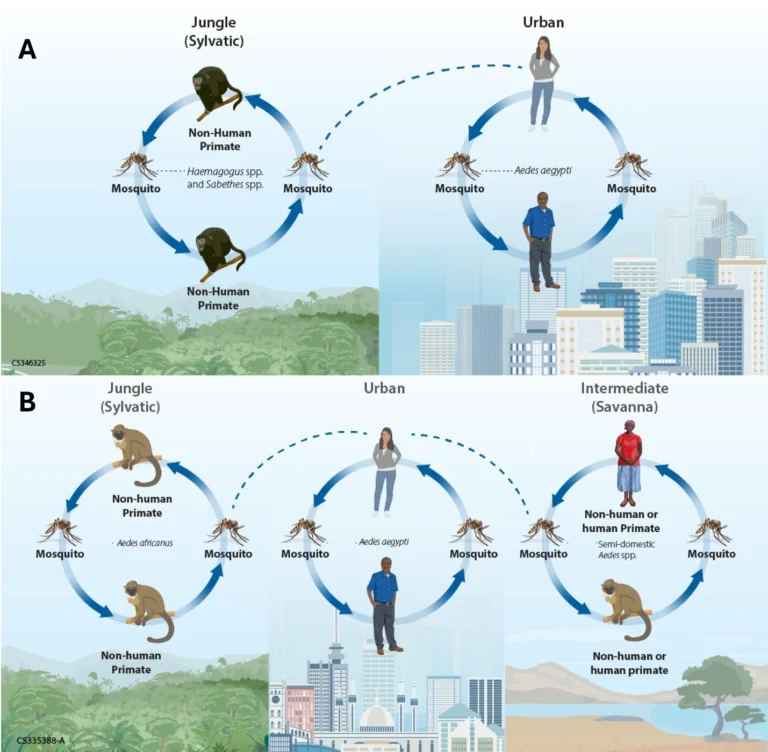
Source: US CDC.
Although yellow fever often presents with mild, flu-like symptoms that resolve in a few days, diagnosis is a challenge given that its clinical presentation mimics other infectious diseases, such as malaria, dengue, and viral hepatitis. Severe disease may occur in a small proportion of patients, affecting the liver, kidneys, and other organs. For 50% of patients that move into this more toxic phase, the disease is fatal. There is no antiviral for yellow fever.
The growing threat of yellow fever
In South America, where the sylvatic cycle is underway, there has been a marked increase in cases. So far this year, 131 cases and 53 deaths have been reported, already exceeding the 61 cases and 30 deaths reported in all of 2024. Most have occurred in Brazil (81 cases and 31 deaths), followed by Colombia and Peru. But due to surveillance challenges, one confirmed case typically indicates about 10 undetected cases.
Illness is almost exclusively among those who are unvaccinated and have had exposure to wild or wooded areas. But experts are particularly concerned about the emergence of yellow fever in previously unexposed areas — where the population would be naive to the virus — and in areas with low vaccine coverage, where previously-unexposed children are likely to be most vulnerable to it.
In this vein, yellow fever’s emergence in Tolima, Colombia indicates new geographic spread, while cases in São Paulo, Brazil risk a larger urban outbreak given the city’s population of more than 22 million. The region’s vaccination rate is only 63%, well below the WHO’s recommended target of 80% for herd immunity.
It was this combination of factors — the spread to non-endemic areas amid low vaccination rates — that led to the region’s last yellow fever epidemic, the largest in the last 50 years, in Brazil from 2016 to 2018. More than 2,100 cases and over 700 deaths were reported as health authorities faced a shortage of the global yellow fever vaccine supply following outbreaks that had recently occurred in Angola and the Democratic Republic of the Congo. Mass vaccination campaigns of fractional doses eventually got the outbreak under control, but it signaled the resurfacing of a long-controlled public health threat.
4 Top Takeaways
- Yellow fever cases multiply across the Americas. The first three months of 2025 have seen 131 cases and 53 deaths of yellow fever in the region, more than double the rates in all of 2024. Cases are likely underestimated as true case counts are at least 10 times what is reported as the virus often goes undetected.
- Expansion of yellow fever to non-endemic areas. Cases have been reported in Brazil, Colombia, Peru, and Bolivia, with many outside of endemic areas. This suggests the arbovirus has undergone geographic spread, increasing the risk of a large outbreak.
- Decreased yellow fever vaccinations drive viral dissemination. Vaccine coverage has declined across the region, largely attributed to insufficient vaccine supply and disrupted immunization programs following the COVID-19 pandemic, meaning larger swaths of the population are susceptible to infection.
- Global vaccine shortages are hampering public health response. Given the sudden need for millions of doses, combined with a limited number of manufacturers worldwide, some regions have resorted to fractional dosing (1/5th of the full dose) to stretch supplies.
Approximately 34 countries in Africa and 13 countries across the Americas are endemic or have areas endemic to yellow fever. Africa bears the brunt of cases, with 13 countries reporting outbreaks between 2023 and 2024. Yet the threat of yellow fever is expected to grow as climate change expands mosquito habitats while globalization and urbanization bring humans closer to infected mosquitoes.
The 2024/2025 Global Incidence of Yellow Fever, January 1, 2024-April 3, 2025
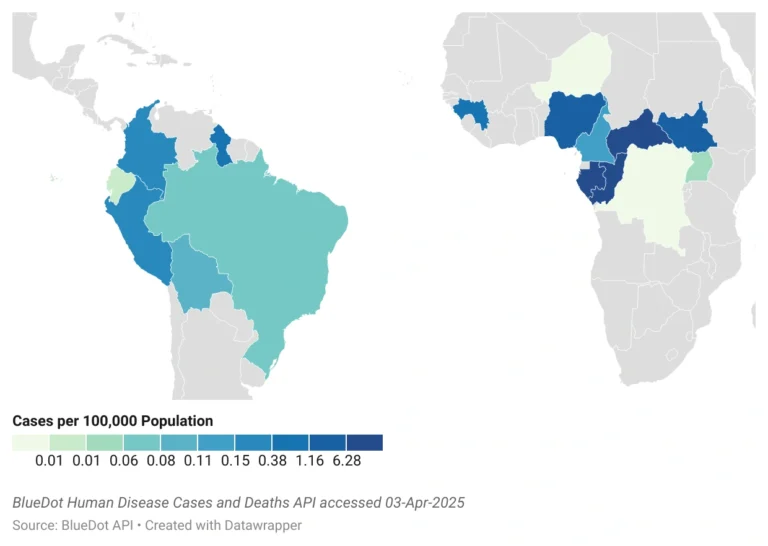
Recent outbreaks also highlight widespread low vaccine coverage — lower than what is needed to prevent outbreaks. The confluence of insufficient vaccine supply due to exhausted stockpiles and manufacturing and storage challenges, disrupted immunization programs, lack of knowledge about the virus and the vaccine, and vaccine hesitancy drives declining immunization rates and increased risk of large-scale outbreaks. Seven of twelve countries with endemic areas in the Americas, including Brazil and Colombia, saw declines in coverage between 2014 and 2023.
Yielding yellow fever transmission
As is the case for several infectious diseases, immunization against yellow fever is the best way to prevent illness. Available for use since the latter 1930s, the yellow fever vaccine has a long history of providing safe, effective, and affordable protection against the virus. Within a month of vaccination, 99% of people achieve lifelong immunity. Additional research is ongoing to develop new vaccines that will help keep up with demand.
Vector control is also vital to limit disease transmission. Using mosquito repellant and wearing long clothing to reduce the risk of getting bitten are important individual-level protection methods, especially when going into forested areas. Robust surveillance systems to track infected mosquito populations and elimination of breeding locations offer population-level prevention beyond vaccination.
Every year, 700,000 people die from vector-borne diseases. As climate change, urbanization, and human movement continue, the risk of these infectious diseases grows. By 2050, nearly 50% of the world’s population are expected to be at risk.
“We can’t easily eradicate yellow fever since it’s zoonotic, and it has a wild animal host” says Dr. Torres Portillo. “But sustained increases in vaccination, along with strengthened tracking and testing, can keep large outbreaks at bay.”
On our radar
- Avian influenza in Mexico: On April 4, Mexico’s Ministry of Health confirmed the country’s first human case of avian influenza A (H5N1). The patient is a 3-year-old girl from the north-central state of Durango, located a four-hour drive from the Mexico-US border, whose economy is based primarily on agriculture and cattle ranching. The child passed away on April 8; the source of the infection remains under investigation while so far no contact with infected animals have been documented.
- Avian influenza in India: Last month, a two-year-old child from Andhra Pradesh died of avian influenza potentially caused by the consumption of raw poultry. Eight avian influenza outbreaks have been reported in Andhra Pradesh in the first three months of the year, resulting in the death or culling of over 600,000 poultry. Human bird flu cases in India are uncommon, but the nation is strengthening its disease prevention strategy.
- Chikungunya in Mayotte: On March 26, the French island territory of Mayotte, near Madagascar, reported its first locally acquired case of chikungunya of the year— its first such case since 2008. This follows three imported cases from the nearby, highly connected French territory of Réunion, which has been battling an outbreak since August last year. Nearby Mauritius also recently reported their first locally acquired case after imported cases were linked to Réunion. Mayotte has activated level 2A of the ORSEC plan to heighten surveillance and response needs.
To learn more about outbreaks as they happen around the globe, sign up here to receive every edition of BlueDot’s biweekly newsletter, Outbreak Insider.









