Spiking cases, unusual clinical presentation, and a heavy disease burden underline the need for countermeasures.
The Indian state of Maharashtra is in the midst of an intensifying — and puzzling — outbreak of chikungunya. The region has reported 3,259 cases of chikungunya since the start of the year, marking a more than fourfold increase from the 790 cases reported by the same time last year — and a notable increase following a few years of low case counts. The city of Pune has been particularly hard hit, with at least 2,000 cases diagnosed.
This particular outbreak has also seen the emergence of potentially atypical and severe symptoms, with an increased number of complications associated with infection. They range from black nose disease and decreased platelet count to encephalitis and even paralysis. While chikungunya is known to cause neurological complications in some patients, these latest manifestations are much less common and may signal a substantially larger outbreak is occurring.
Evidence suggests that the current outbreak is attributable to a resurgence of the known Indian Ocean strain, but viral changes or mutations could also be having an impact. “We need to determine if there have been any genetic changes in the virus that can impact its ability to infect, cause severe disease, spread easily, and evade the immune system,” says BlueDot Head of Surveillance Dr. Mariana Torres Portillo.
This latest outbreak underscores the fact that containing chikungunya is an international public health challenge — one that has been taken up by the pharmaceutical industry. One vaccine is now approved in North America and Europe, while others are in the late stages of development.
The Chikungunya Chronicles: A Brief History
Chikungunya is a mosquito-borne illness caused by an RNA virus of the Togaviridae family. Like dengue and Zika, chikungunya is an arbovirus primarily transmitted by Aedes aegypti and Aedes albopictus mosquitoes. Since its discovery in Tanzania, Africa in 1952, chikungunya has spread to nearly every continent, with cases reported in at least 118 countries. Its increased dissemination, as with other vector-borne diseases, is largely driven by factors like climate change, human and animal mobility and behaviour, deforestation, and land use.
Today the highest number of reported chikungunya cases are found in the Americas, where it first arrived only 11 years ago. A recent BlueDot Intelligence Report found that the region saw nearly 300,000 cases and 300 deaths between January and July 2023, totaling more than 720,000 cases since 2020 (see image). Brazil has reported the highest number of cases, with over 1 million total between January 2019 and July 2024. Following behind is India at nearly 370,000 cases — a number rapidly increasing due to the current outbreak.
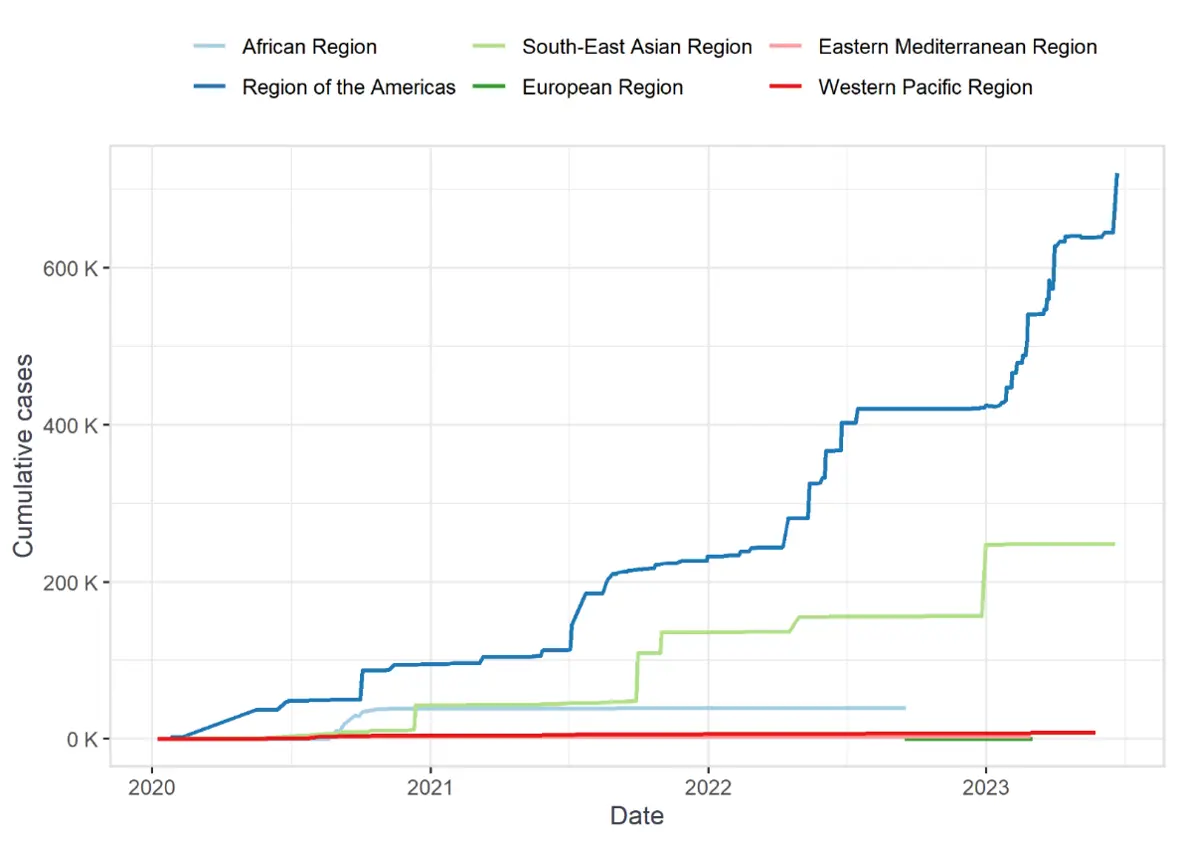
Source: BlueDot Intelligence Report, August 2023
Chikungunya activity is often sporadic in endemic areas across Africa, Asia, and the Americas. Major epidemics appear to follow a cyclical pattern, whereby infection erupts in non-immune populations before lying dormant for about 7-8 years — though sometimes as long as 20 years. During these interepidemic periods of the transmission cycle in humans, the virus is conserved through an enzootic cycle, meaning it is continuously transmitted between mosquitoes and wild animals, including bats, birds, and numerous species of non-human primates.
Most of chikungunya’s symptoms — abrupt onset of fever, headaches, and muscle pain — all overlap with other arboviruses such as dengue and Zika, which result in considerable diagnostic challenges and a lack of clarity on the true burden of the disease. This is believed to be the case with the current outbreak in India, where chikungunya is among several infectious diseases, alongside malaria and dengue, that have stricken the country this year.
A Burdensome Disease
The hallmark symptom that sets chikungunya apart from other arboviruses is significant joint pain; its name is derived from the Kimakonde word for “to become contorted“. Most symptoms typically emerge within 3-7 days post-bite and resolve within a week. Evidence suggests that infection can result in long-term, and potentially lifelong, immunity.
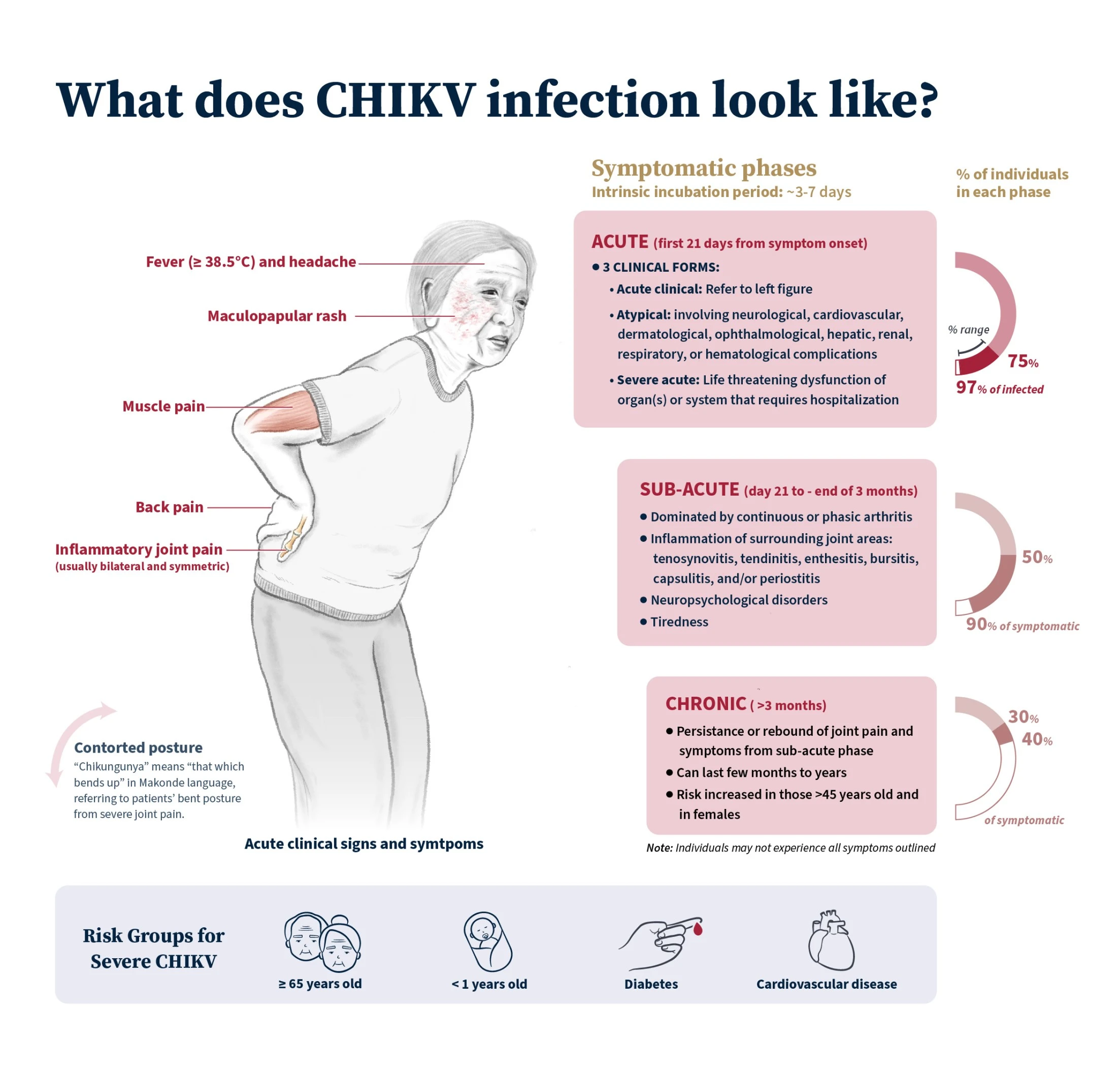
Source: BlueDot Intelligence Report, August 2023
However, up to 40% of those infected experience chronic joint pain that can last years. Chikungunya also carries risk of more severe disease to certain groups, particularly for newborns, older adults (≥65 years), and those with medical conditions (such as heart disease and diabetes), which can lead to cardiovascular and neurological complications, including myocarditis, encephalitis, and Guillain-Barré syndrome.
Deaths associated with infection are considered rare (<1%), though they may be underestimated. Chikungunya virus infection is associated with a significant disease burden due to its wide geographic distribution, frequent outbreaks, and the long-term symptoms that can occur following infection. Globally, chikungunya was associated with an estimated 106,089 disability-adjusted life-years (the number of years lost due to morbidity and mortality) annually between 2010 and 2019. Chronic complications were the primary drivers of the overall disease burden, far outweighing the burden of acute infection. Treatment usually involves managing symptoms with antipyretics and analgesics, as well as disease-modifying antirheumatic drugs (DMARDs) in chronic cases.
4 Top Takeaways
- Chikungunya cases are climbing in western India. Maharashtra, the second-most populated state in India, has recorded fourfold higher case counts in 2024 compared to the same time last year.
- Peculiar presentation may point to mutations in the virus. Atypical — and more severe — symptoms and complications have been reported, including black nose disease and encephalitis, signaling potential mutations in the virus.
- Chikungunya is vastly underdiagnosed and carries a high burden. Up to 40% of patients develop chronic symptoms, with substantial impact on quality of life. With considerable surveillance and diagnostic challenges, the true burden of infection and complications incidence is unclear.
- Available vaccines for the virus are on the horizon. Chikungunya vaccines are increasingly being developed and could be an important countermeasure against infection and spread — especially for endemic countries
Countering Chikungunya
Nearly 4 billion people — approximately 39% of the global population — are at risk of chikungunya infection. Recent BlueDot analyses have found that chikungunya outbreaks are on the rise around the world, though they often go undeclared or have delayed communications due to challenges with surveillance. As climate change expands mosquitoes’ environments and seasonal activity, the threat to populations in endemic and nonendemic regions is growing rapidly, which has spurred vaccine development.
To date, Valneva’s chikungunya vaccine is the only one approved in North America and Europe, and regulatory reviews are underway in the UK and Brazil. Several other vaccine candidates are in various stages of development and regulatory review, including those of Bavarian Nordic and Emergent BioSolutions. Making vaccines readily available in countries with heightened risk is vital for reducing disease burden.
As more data are gathered, research will confirm the long-term safety of vaccine candidates and address key questions that will assist health authorities in planning vaccine deployment strategies. These questions include whether the vaccines should be included in routine immunization programs or used as outbreak response vaccines in endemic countries, the quantities of vaccine required in these scenarios, and how to ensure adequate vaccine procurement, particularly for vulnerable populations.
“Chikungunya is underreported and we know it can cause complications, but we really don’t understand the true burden of the virus,” says Dr. Torres Portillo. “There are very few studies on the neurological manifestations and other complications associated with the disease. That makes it ripe for further research so we can better understand it and continue to grow our armamentarium — from vaccines to treatments targeting the prevention of chronic joint pain and complications derived from the infection”.
On Our Radar
- Bird flu testing in Missouri: Blood samples from five healthcare workers are being tested for bird flu this week. The workers developed respiratory symptoms while caring for a patient infected with H5N1. A sixth healthcare worker also reported symptoms, but their test came back negative for H5N1, meaning their symptoms were likely caused by another infection such as COVID-19.
- Eastern equine encephalitis: A resident of New York State died of this mosquito-borne disease in late September. Rare but endemic, the disease has been top of mind across the northeastern United States this summer, as some communities closed parks at night and warned residents to stay inside.
- Oropouche virus: Our latest peer-reviewed publication accurately predicted Florida and New York as key destinations for travelers infected with Oropouche, a virus Outbreak Insider first covered back in June. Additional locations, including Spain and England, are also at risk. Explore the full paper here.
To keep updated on chikungunya and other infectious disease outbreaks around the globe, sign up here to receive every edition of BlueDot Outbreak Insider.









