Three battles we fought — and another we won — against emerging threats and resurgent foes over the past year
From unexpected outbreaks that challenged global health systems to groundbreaking advancements in disease surveillance and prevention, this past year has been a whirlwind of activity in the world of infectious diseases and disease prevention.
Widespread cases of chikungunya, avian influenza, and cholera emerged in the midst of a warming climate and ongoing regional conflicts. Vaccine-preventable diseases such as measles and pertussis resurfaced — the long tail of the fallout from both COVID-19-related disruptions to vaccine programs and vaccine hesitancy. At the same time, enhanced public health measures saw severe diseases like Ebola rapidly contained before mass devastation occurred.
“Not everything we saw came as a surprise,” says Andrea Thomas, BlueDot’s head of epidemiology. “Reflecting on this year reminds us that the battle against infectious diseases is never truly over.”
This edition of Outbreak Insider covers strides made, setbacks faced, and barriers overcome in 2025, and what to look out for in 2026.
Evading an Ebola emergency
On September 3, a reported unknown hemorrhagic illness resulted in the deaths of eight people in the Democratic Republic of the Congo (DRC). The next day, the outbreak was confirmed as Ebola, a rare but often fatal illness first detected in 1976. It marked the DRC’s 16th recorded outbreak since Ebola’s discovery, but genomic sequencing identified that the strain more closely resembled the 1976 strain, indicating a new zoonotic spillover event between animals and humans.
The risk of uncontained community spread was high. But by the end of September, thanks to immediate community outreach, rapid deployment of medical teams and countermeasures including vaccines and personal protective equipment (PPE), cases had waned. On December 1, the outbreak was declared over following 42 consecutive days without a new case.
“Controlling an Ebola outbreak in three months is an inspiring example of the power of collaborative, multi-sectoral response,” says Dr. Mariana Torres Portillo, BlueDot’s head of surveillance. In total, 64 cases and 45 deaths were reported. While these outcomes are tragic, the decisive actions taken were crucial in preventing the disease from spreading further, saving countless lives.
Wins such as this do not always occur because of longstanding inequities in access to available countermeasures. Countries such as the DRC often rely on global support to bolster country-level systems and expertise, especially in resource-limited locations. But when these challenges are overcome, they are beacons for what public health agencies and workers can accomplish.
Setbacks on the frontlines
Where gaps exist and ability to respond is impaired, infectious diseases can thrive. This year, cholera, an acute diarrheal illness, was the old adversary that resurged in Africa and the Middle East. Severely damaged infrastructure and poorly resourced health systems in humanitarian crisis zones created an inaccessibility to safe water, sanitation, and hygiene, as well as delayed access to treatment, producing ideal conditions for the bacteria to thrive.
A total of 565,404 cases and 7,074 deaths have been reported across 32 countries this year, largely in Africa, but also across parts of the Middle East and South Asia. Africa is in the midst of its worst outbreak in 25 years as cases and deaths exceed 311,000 and 7,000, respectively. The hardest hit nations are South Sudan (78,034 cases), Sudan (72,000), the DRC (63,521), and Angola (35,163), which together account for approximately 85% of deaths, according to the latest Africa Centres for Disease Control and Prevention (CDC) weekly report.
Cholera and AWD cases per 100,000, Jan. 1-Oct. 26, 2025
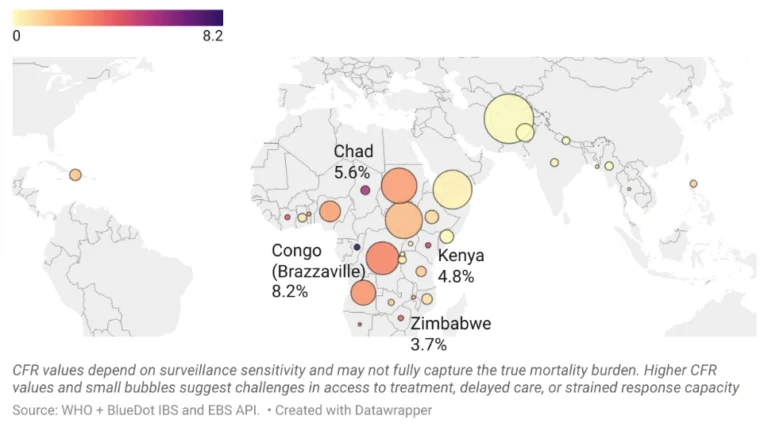
Source: World Health Organization, Multi-country Outbreak of Cholera External Situation Report n. 32, published November 26, 2025.
Afghanistan and Yemen combined have seen more than 233,000 cases of cholera and acute watery diarrhea (AWD) in 2025. For nations in all these regions, conflict and natural disasters have caused destruction, mass displacement, and overcrowding. Combined with limited oral cholera vaccine (OCV) supply and challenges to timely delivery, 1 billion people are at risk of infection. Efforts to combat this long-time foe, such as the Global Roadmap to End Cholera by 2030, offer guidance and hope in achieving victory.
Another old foe of public health also made a resurgence in 2025 — despite having the tools necessary to fight it. Measles, the highly contagious, vaccine-preventable respiratory virus resurged in regions that typically do not see uncontrolled spread. Approximately 492,000 cases have been reported so far this year, compared to 475,000 cases last year. Since 2021, the number of countries experiencing large measles outbreaks has tripled. And while measles deaths have fallen since 2000, an estimated 95,000 deaths in 2024, mostly among children under 5, underscore a painful truth: children are still dying from a disease we can prevent.
The spread of measles is driven by immunization gaps, which have been exacerbated by pandemic-related disruptions and increased vaccine hesitancy. Access to and distribution of the highly effective vaccine remains an issue for some areas. For others, a decline in immunization — often the result of misinformation or lack of trust — was the culprit. In the Americas, where measles vaccines are widely available, first- and second-dose vaccination rates were 88% and 77%, respectively, dropping below the recommended threshold of 95%. Communities with lower immunization proved particularly vulnerable to importation and circulation.
Measles Incidence in 2025 and Vaccination Coverage with a Second Dose of Measles-Containing Vaccine for 2024, January 1 to December 15, 2025
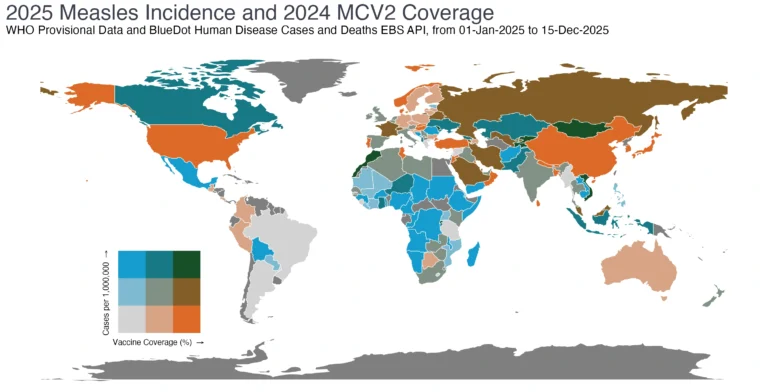
Data from BlueDot Human Disease Case and Death Counts API and WHO Immunization Data Portal, accessed December 15, 2025. Source: BlueDot 2025 Measles Report
Last month, Canada lost its nearly 30-year measles-free status as cases surpassed 5,200. The US and Mexico are at risk of losing their elimination statuses early in the new year. “Barriers to widespread vaccination, whether it be for cholera in conflict zones or measles in vaccine-hesitant communities, have far-reaching implications for diseases we’ve been waging war with for a very long time,” says Torres Portillo.
If there is a silver lining to measles’ resurgence, it’s to be found in Africa. The continent made substantial headway in measles immunization: first-dose rates hit 71% in 2024, up 50% from 2000; second-dose rates hit 55% in 2024, a 1000% increase from just 5% in 2000. In the same timeframe, there has been a 40% decrease in cases and 50% reduction in deaths.
This year also saw a less anticipated but dominant infectious disease opponent: arboviruses. Mosquito-borne diseases like chikungunya soared, evidenced by the 44 alerts sent out by BlueDot since January. This once regional disease is now a global one, with more than 445,000 chikungunya cases and 155 deaths reported across 40 countries as of the end of September. Cases not only spiked in endemic countries including Sri Lanka and Brazil, but the disease also reemerged on the islands of Réunion, Mayotte, and Mauritius and began circulating locally for the first time in China, France, and the US.
Global chikungunya outbreak status and total reported cases, Jan. 1, 2024-Dec. 10, 2025
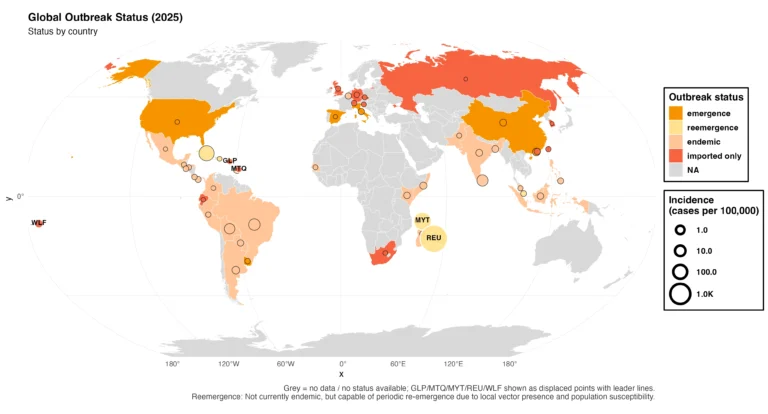
Note: Grey = no data/no status available. “Reemergence” indicates cases that are not currently endemic but are capable of periodic reemergence due to local vector presence and population susceptibility.
Data Source: BlueDot Human Cases and Death API and PAHO Chikungunya analysis by country, accessed 10-Dec-2025. Note: Population size of countries is from 2021–2022.
The widespread surge in mosquito-borne diseases is influenced by climate change, which has been shown to aggravate nearly 60% of infectious diseases. For example, warmer weather and altered rainfall in Europe are creating the perfect environment for chikungunya-carrying mosquitoes to flourish. The Aedes albopictus mosquito is now established in 16 European countries, meaning outbreaks of mosquito-borne diseases are becoming the norm. By the end of August, the continent had recorded 27 chikungunya outbreaks. It also recorded the highest number of West Nile virus cases in three years. The expansion of suitable habitats and longer seasons for infectious disease-carrying vectors is likely to lead to more outbreaks around the globe.
The emergence of chikungunya in new areas is not just an artefact of climate change; it is linked to increased human movement and connectivity, as travelers can introduce diseases and vectors can hitch rides to new land. Travel-associated cases, along with vector presence and environmental suitability, can ultimately lead to local transmission. This series of events is what led to this year’s outbreak in Guangdong, China, which resulted in over 16,000 cases. Importation also catalyzed the outbreaks in France, Italy, and the US.
3 Top Takeaways from 2025
- Ebola is proof that preparedness pays off. Detection of the highly fatal and difficult-to-contain hemorrhagic disease in the DRC in early September sent warnings of a potentially devastating outbreak. But rapid, multi-sectoral action ushered in the end of the outbreak on December 1.
- Infectious disease battles engaged combatants old and new. Cholera, measles, and chikungunya dominated, exposing gaps in basic sanitation, immunization, and surveillance. Conflict, climate change, human movement, and reduced immunizations were catalysts for disease transmission.
- New year, new battleground. Environmental and socio-political pressures mean diseases like avian influenza, polio, and tick-borne diseases are threats to watch in 2026. But with advancements in artificial intelligence and machine learning, timelier surveillance provides hope for improved time to action.
Global outbreaks exposed inadequate surveillance and reporting of mosquito-borne diseases. Outbreaks are often reported retrospectively, resulting in significant delays in outbreak communications and initiation of important prevention measures. In a recent BlueDot analysis, there was a median 79-day lag between outbreak detection and official outbreak declarations or advisories in 2025 — vastly longer than BlueDot’s median 3-day lag. And only 56% of chikungunya outbreaks were declared by major health agencies, while nearly 30% went completely undeclared.
These delays in official reporting, combined with the propensity for travel-related importation, have led many sub-national public health agencies to follow their own lead, seeking out alternate intelligence sources such as BlueDot and taking steps to mitigate travel-related spread before official announcements are made.
Start the new year by getting ahead of emerging threats
Our intelligence platform tracks and verifies emerging health threats worldwide, delivering near real-time, expert-reviewed insights tailored to your organization.
Register for a one-month free trial of BlueDot’s Event Alerts and Personalized Briefs.
Get ahead now— click here to sign up.
Forecasting infectious diseases in 2026
In the year ahead, BlueDot will be closely monitoring several infectious diseases — including some that made headlines and worried experts, and others that flew beneath the radar. Among the questions looming for 2025:
- Will avian influenza continue to spread widely in many species, increasing the likelihood that a human-adapted strain could emerge?
- Can catch-up initiatives restore immunization rates for measles and other vaccine-preventable illnesses like polio and pertussis?
- How will climate change and other factors impact the burden of vector-borne diseases, whether spread by ticks, mosquitoes, or other insects?
As artificial intelligence and machine learning rapidly advance, so too will disease detection, diagnosis, and risk assessments. Knowledge is power and knowing when and where outbreaks are circulating is going to be key in navigating the challenge of tracking infectious diseases in an increasingly fragmented but highly connected world.
Stay ahead of what’s next
Infectious disease risks will continue to evolve in 2026, making timely and trusted intelligence critical for preparedness and response. BlueDot delivers near real-time disease data and expert-reviewed insights in an easy-to-use platform to help you understand where outbreaks are emerging, how risks are changing, and what to watch in the year ahead.
Learn how BlueDot supports early detection and informed decision-making.
Barriers to infectious diseases may not be disappearing anytime soon, but the tools to quickly identify and initiate prevention measures provide hope in reducing infectious disease burden in 2026.
In our interconnected and rapidly changing world, the threats posed by global infectious diseases are only increasing,” says BlueDot founder and CEO Kamran Khan. “But the technologies and solutions needed to quickly identify, assess, and respond to them are also advancing quickly. Leveraging these innovations is mission critical to strengthening organizational readiness and resilience in 2026 and beyond.”
On our radar
- Novel mammarenavirus-like infection in Chad: On November 13, a new mammarenavirus was reported in a 37-year-old male with recent travel to Chad. Lab testing confirmed the pathogen was not Lassa virus, and the mode of transmission is unknown. Symptoms are severe, yet distinct, and the emergence of this new pathogen in an under-surveilled region is fueling investigation to mitigate broad exposure and identify potential viral hosts.
- Marburg in Ethiopia: As of November 26, 13 cases and 8 deaths from Marburg have been reported in Ethiopia. The nation’s first historical outbreak of the disease, which was confirmed on November 14 in Jinka, has now spread to Hawassa — over 500km away. The source is not yet known, raising concerns about the risk of further spread within and across borders. Public health measures are rapidly gaining strength to track and limit infection, including a clinical trial with 640 doses of an investigational Marburg vaccine developed by the Sabin Vaccine Institute.
- H5N2 in Mexico: A case of avian influenza(H5) reported on October 2 in Mexico City was confirmed a novel highly pathogenic reassortant strain of H5N2. A combination of clade 2.3.4.4b A(H5N1) and low pathogenic avian influenza (LPAI) A(H5N2), the strain shows mutations that may have resulted from mammalian adaptation during the human infection. This case marks the third human infection of influenza A(H5) in Mexico, amounting to 75 human cases reported across the Americas since 2022.
As Outbreak Insider winds down for the holiday season, BlueDot’s work will not. To keep up-to-date on outbreaks and expert insights, sign up here. We’ll see you in the new year for the latest in infectious disease news. Wishing you a healthy and happy holiday!









