North America teeters on the edge of losing measles-free status, proving that disease elimination is not a finish line but a maintenance task
Next Monday, October 27, Canada will lose its measles elimination status, a designation it has held for almost 30 years, due to a sustained series of measles outbreaks in the past year. For similar reasons, both the United States and Mexico are also at risk of losing their measles-free status in the months ahead.
North America’s outbreaks are part of a measles resurgence that has erupted around the globe. More than 425,000 cases and 1,800 deaths have been reported to date in 2025, with an upward trend on track to surpass last year’s 475,000 total cases. In the Americas, measles cases are 25-fold higher than the same period last year, as of October 21.
“This wouldn’t be the first time a country has lost, or nearly lost, its measles-free status,” said Dr. Mariana Torres Portillo, BlueDot’s head of surveillance. At the same time, several countries have managed to regain control after significant outbreaks, and some have successfully restored their measles-free status. “Hope is not lost. What we want to avoid now is seeing measles become endemic again in the Americas, and the key is to increase vaccine coverage.”
This edition of Outbreak Insider takes a closer look at North America’s continued disease transmission, how other countries have regained control of outbreaks, and how BlueDot’s connectivity analyses offer key insights to mitigate risk.
From elimination to escalation: North America’s measles revival
Measles is a human-only viral infection that is transmitted by respiratory droplets. It is considered one of the world’s most contagious infectious diseases: one contagious person can infect 12-18 others. Approximately 40% of those with measles are hospitalized, and for some the disease can be fatal, notably for children who are as yet unvaccinated. Before the vaccine was available, epidemics were frequent, and 2.6 million lives were lost each year.
In Canada, measles was considered eliminated in 1998 following mass immunization. From 1998 to 2024 Canada averaged a mere 91 measles cases per year, with any outbreaks swiftly brought under control. But in October 2024, a single imported case from a returning traveler set off a chain reaction: the country has since recorded more than 5,000 cases and two deaths, more than in the previous 27 years combined, making Canada among the top countries reporting measles worldwide. In the United States, a total of 44 outbreaks and 1,596 cases have been reported to date in 2025, significantly fewer than Canada, but still a five-fold increase over the 285 cases the U.S. reported last year.
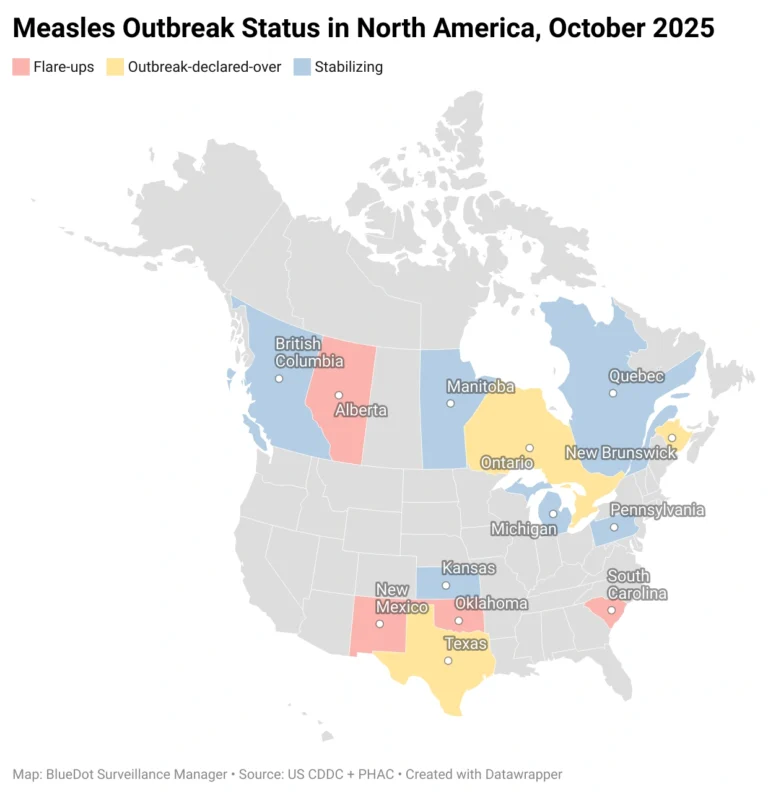
While each country’s original outbreaks (in Texas for the U.S., in New Brunswick and Ontario for Canada) has been declared over, others states and provinces are still working to either stabilize previous outbreaks or manage recent flare-ups.
Outbreaks are largely due to declining vaccine coverage — both countries’ vaccination rates have fallen below the 95% threshold needed to prevent outbreaks — and fueled by local transmission. Approximately 95% of Canada’s cases are among people who are unvaccinated, under-vaccinated, or with unknown vaccination status. The country’s first- and second-dose vaccination rates were 92% and 79%, respectively, in 2024 — substantially below the 95% threshold needed to prevent outbreaks.
Where coverage falters, measles flares
On a global scale, incidence of measles largely coincides with low vaccination coverage. Countries with high vaccination coverage, such as China, Norway, Sri Lanka, and Türkiye, have low incidence of measles. Likewise, countries with low vaccine coverage, including Cambodia, Mexico, Nigeria, and Romania, have high incidence.
Measles Incidence in 2025 and Vaccination Coverage with a Second Dose of Measles-Containing Vaccine for 2024, January 1 to October 21, 2025
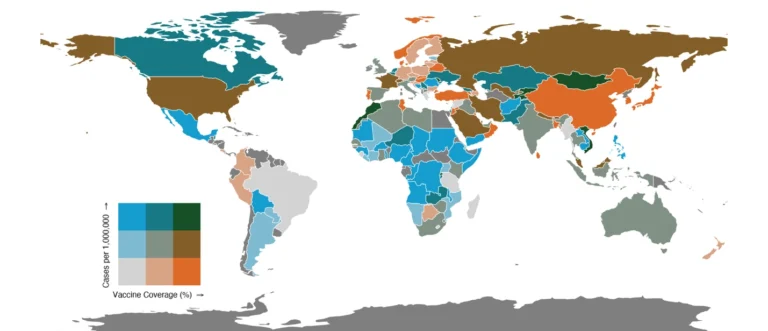
Source: Data from BlueDot Human Disease Case and Death Counts API and WHO Immunization Data Portal, accessed Oct. 21, 2025.
There are also countries with low vaccination coverage (46-75%) and low incidence of disease, such as Brazil and Greece, as well as countries that have not reported any measles cases so far this year, including the Bahamas and Fiji — all of which are at risk of a measles resurgence given the disease’s increased global activity. Yet some countries, like Morocco, Mongolia, and Vietnam, have — like Canada — reported many new cases despite relatively high vaccination coverage. These cases exemplify the challenge of a disease as contagious as measles, which can spread quickly in any pockets of the population with suboptimal immunity.
Despite the challenge of controlling measles, there have been success stories. Since late 2023, Morocco has been battling an intense measles outbreak that has infected more than 25,000 people. In response, public health authorities initiated a mass vaccination campaign in March 2024 to fill immunization gaps. By April this year, focusing on the country’s 10.8 million people under age 18, Morocco had brought the national immunization rate above 98%. The benefits of this public health feat were immediate, with the country reporting an 80% reduction in measles incidence by May 2025.
Other countries have regained measles elimination status owing to enormous efforts to strengthen surveillance and preventive measures. Last November, Brazil was re-verified as measles-free after losing this status in early 2019 when an outbreak infected 21,700 people. Further, some countries have achieved or maintained measles-free status. Earlier this year, the WHO announced that all 21 Pacific Island countries had eliminated both measles and rubella. In 2016, Hong Kong was declared measles-free and has remained so amid a decade of concurrent outbreaks that threatened immunization programs. The key factor in the country’s success has been its consistently high two-dose coverage.
“There are no two ways about it, high immunization rates are the gold standard to prevent measles outbreaks,” says Dr. Torres Portillo. Since it was introduced, the measles vaccine has prevented tens of millions of deaths. It has been proven safe and effective, warding off almost 100% of illnesses and offering lifelong immunity.
3 Top Takeaways
- Canada is on the cusp of forfeiting its measles-free status. Following a year of continuous transmission, Canada is close to losing a designation it’s held since 1998. The country has reported more than 5,000 cases and two deaths in 2025 to date.
- Increased immunization brings outbreaks under control. Nearly 425,000 measles cases and 1,800 deaths have been reported around the globe so far this year. To contain disease resurgence, closing the immunization gap is crucial — and possible with a nearly 100% effective vaccine.
- Endeavouring to achieve measles elimination. Low vaccination rates in communities around the world raise the risk for local, national, and international disease spread. Effective surveillance helps identify where outbreaks are occurring to initiate rapid response, minimize disease impact, and move the needle toward measles eradication.
Calculating connectivity
In the effort to eliminate measles, strong surveillance is the second-most important factor. With it, outbreaks can be quickly detected and contained. And with such high global connectivity, the risk of imported cases is significant — and heightened by the sustained outbreaks in the Americas, which have high connectivity with many other parts of the world. Depending on the timeliness and effectiveness of the response, introducing measles into a population of unimmunized people could have devastating effects.
For instance, Brazil’s population exceeds 210 million, and the country welcomed nearly 5 million visitors between January and May this year alone. Yet Brazil’s second-dose vaccine coverage in 2024 was only 68%, creating a substantial risk for outbreaks and the loss of their newly acquired measles-free status. Though much smaller in population (approximately 400,000), the Bahamas — a travel hotspot — saw a record-breaking 11 million visitors last year and only had 60% second-dose coverage.
Quantifying importation risk would help countries like Brazil and the Bahamas take the steps necessary to minimize outbreaks. By combining event-based and indicator-based surveillance with travel connectivity, BlueDot can map air and ground travel, allowing for prioritization and triage of locations most at risk of importation. This method accurately predicted measles transmission from the United States to the U.S.-Mexico border.
What does your region’s risk map look like?
BlueDot’s analysis of air and ground connectivity shows the travel linkages for any region, demonstrating where and when travelers arrive from different parts of the world — and the infectious diseases they’re most likely to bring with them. Contact us to learn more.
“One travel-related case in Canada opened the flood gates to a cascade of outbreaks that public health practitioners are still trying to control,” says Dr. Torres Portillo. Peak travel season is coming up in the United States, with thanksgiving get-togethers sending millions of travelers onto the road and into the skies for the holidays. Bookings in the US are already up 2% compared to last year, when an estimated 80 million travelers broke the nation’s record for air travel. Knowing where outbreaks are happening and how connected to them travelers are can protect at-risk populations — and help eliminate measles around the world.
On our radar
- Heartland Virus in the USA: Heartland virus, an underreported but emerging tick-borne disease, was reported on October 15 in Missouri — the state’s first case this year. The disease is primarily transmitted by the Lone Star tick, which hitches rides on wild mammals across the southeastern and midwestern US. Heartland virus causes non-specific flu-like symptoms but can lead to hospitalization in some cases. Like most tick-borne diseases, Heartland virus likely goes undetected and undocumented in cases that are not severe, impairing an understanding of its severity and true activity.
- Lyme disease in Slovakia: Another more well-known tick-borne disease has shown a substantial increase in the central European country. As of September 17, 3,127 cases of Lyme disease have been reported so far this year. Nearly three times higher than previous years’ averages, climate-related changes and limited prevention options are providing the ideal environment for disease transmission, with broader regional risk.
- Chikungunya in New York: On October 14, 2025, New York State confirmed its first locally acquired case of chikungunya, a mosquito-borne virus, in a woman from Long Island with no travel history outside the state. This marks a significant milestone because it suggests that local mosquitoes—particularly Aedes albopictus, a species now established in parts of New York—may be capable of transmitting the virus for the first time in this northerly location. While health officials classify the risk as low and believe this to be an isolated case, it highlights how climate change, urbanization, and global travel are creating conditions for tropical diseases to appear in new regions.
Estimating risk of infectious disease transmission using BlueDot’s novel technique that integrates surveillance data and location connectivity by air and ground travel provides public health practitioners and healthcare professionals with the information necessary to prioritize their efforts to minimize disease impact.
To receive outbreak intelligence and expert insights, sign up here to receive every edition of BlueDot’s newsletter, Outbreak Insider.









