This week marks the start of the Hajj, the annual pilgrimage to Mecca, which begs the question: How do you keep 3 million visitors safe from infectious disease?
From June 4 to 9, the annual religious pilgrimage to Mecca, Saudi Arabia known as the Hajj will take place. One of the world’s largest annual mass gatherings, this year’s pilgrimage is expected to receive approximately 2-3 million people. It’s among human civilization’s most distinguished religious celebrations. It’s also a public health conundrum.
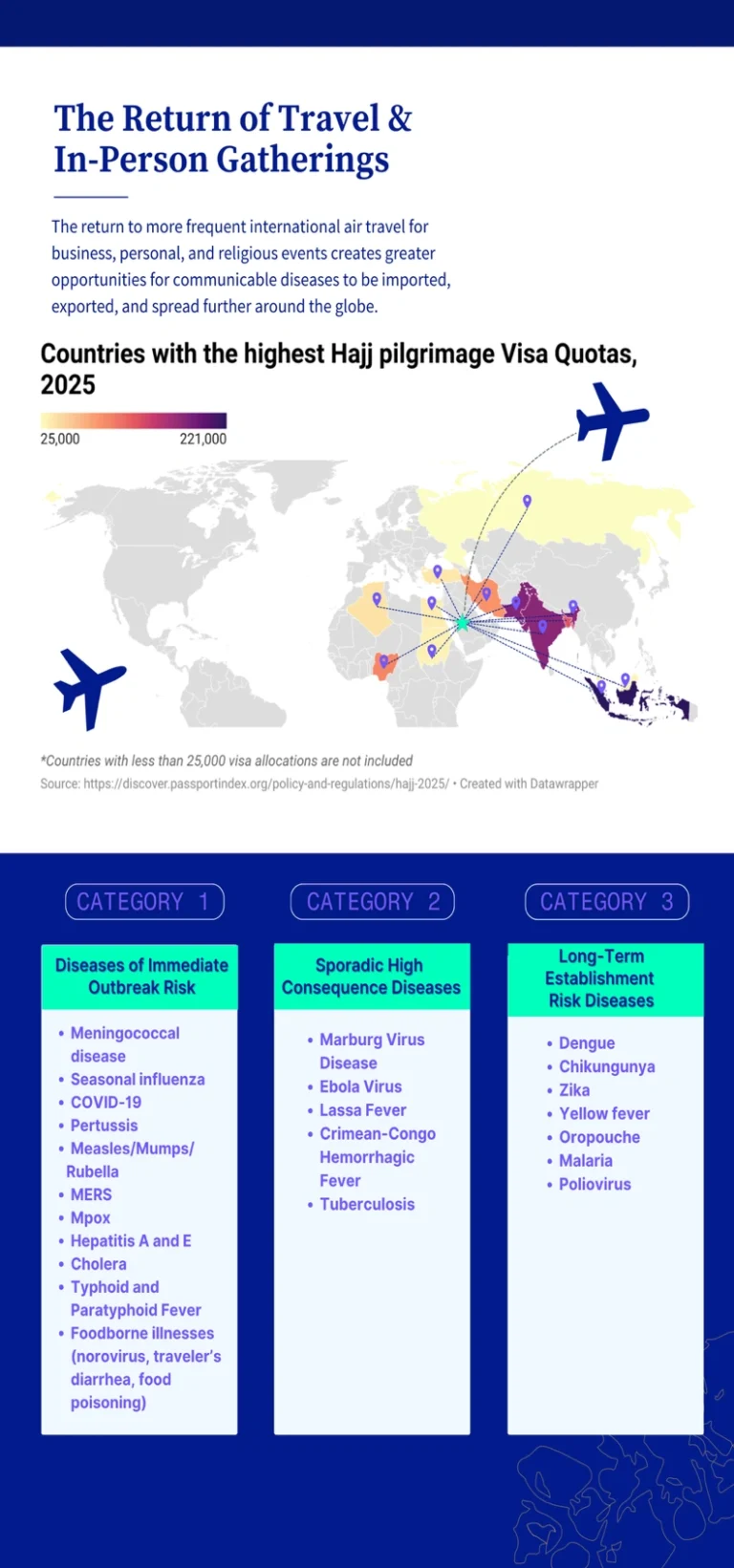
Mass gatherings such as the Hajj invariably entail crowded spaces, sanitation challenges, and hygiene concerns as host locations welcome visitors from around the world, which combine to increase the risk for infectious disease outbreaks. Some 88% of Hajj participants will travel into Saudi Arabia from foreign countries, each with varying vaccination requirements and uptake rates. Respiratory infections, meningococcal disease, and food-, water-, and vector-borne illnesses are no strangers to such events.
Preventing outbreaks in these settings is a complex, collaborative, and lengthy effort often involving local and international organizations, with extensive, effective, and minimally disruptive measures to abate public health hazards. “The Hajj serves as an example of a mass gathering event with strong public health precautions,” says Andrea Thomas, PhD, head of epidemiology at BlueDot, which has conducted risk assessments for previous Hajj pilgrimages, the 2022 FIFA World Cup in Qatar, and the 2020 Olympics held in Tokyo. “There’s a lot to be learned from how risk is managed.”
Mass gatherings manufacture increased risk for infectious diseases
Be they religious celebrations, music festivals, business conventions, or sports tournaments, mass gatherings encompass any spontaneous or organized event that brings together a population large enough to potentially strain local resources and affect emergency response capacity. Each one presents many health hazards and places unique pressures on the host location, notably for respiratory and gastrointestinal tract infections. The 2002 and 2008 Lourdes pilgrimages in France, which had a cumulative attendance of 5 million and 8 million, respectively, both resulted in a norovirus outbreak. And earlier this year, more than 600 million people attended the 45-day Maha Kumbh Mela in India to take a sacred bath in the Triveni Sangam, which has historically been associated with cholera. More recently, the Kumbh Mela pilgrimage has also been linked to the spread of COVID-19.
Respiratory infections, including COVID-19, influenza, and measles, are easily transmitted in confined spaces, especially in environments with poor ventilation and cool and dry air. Gastrointestinal infections, such as norovirus, Salmonella, and hepatitis A may emerge from unsanitary environments, as well as unhygienic food preparation and contaminated food.
Transmission of infectious diseases may be of immediate, sporadic, or long-term risk. Factors such as the type of event, environment, and location need to be evaluated to assess the level of risk for infectious diseases to spread. The risk of COVID-19 notably led to delaying the 2020 Tokyo Olympic games for a full year, and to a ban on spectators when the games were finally held. But despite the complexities of mass gatherings, outbreak prevention can be accomplished with far less stringent measures.
3 Top Takeaways
- Mass gatherings magnify infectious disease risk. From sporting events like the Olympics to religious pilgrimages like the Hajj, events that bring many people together have the potential to become superspreader events for several infectious diseases, including respiratory and gastrointestinal infections.
- Risk remains during and after the event. Infectious diseases may present immediate risk of transmission, be sporadic but high-consequence, or emerge as a long-term risk.
- Public health preparedness is imperative. Gearing up for mass gatherings with updated immunization requirements for attendees, reinforced surveillance and diagnosis capacity, and expanded healthcare services are some ways to limit infectious disease transmission and severe illness.
Case Study: How infectious disease risk is controlled during the Hajj in Saudi Arabia
With many decades of experience in local and international collaboration, the Hajj serves as a prime example of implementing preventive health measures during mass gatherings. Saudi Arabia has advanced its healthcare infrastructure, and annual Hajj preparation kicks off months in advance.
Managing infectious diseases begins with a risk assessment for outbreaks based on import and export potential. Officials gather information about where attendees are coming from to assess the potential infectious diseases to monitor. Since Saudi Arabia regulates participation in the Hajj through country-specific quotas, this is more easily tracked. The countries with the highest quotas for this year are Indonesia (221,000), Pakistan (179,000), India (175,025), Bangladesh (127,198), and Nigeria (95,000).
Utilizing internal and external data on endemic diseases and recently reported outbreaks, BlueDot classifies infectious diseases by risk of immediate transmission during the Hajj, by those that have high consequence but are typically reported sporadically, and by those that pose risk of long-term establishment in Saudi Arabia. Disease transmission pathways are then narrowed down in order to promote protective measures. Some infectious diseases of concern for this year’s Hajj include meningococcal disease, measles, dengue, COVID, malaria, cholera, Crimean-Congo hemorrhagic fever (CCHF), yellow fever, Middle East Respiratory Syndrome (MERS), pertussis, and seasonal influenza. See the figure below for further examples.
Vaccination programs play a critical role in infectious disease prevention. Leading up to the Hajj, those planning to participate in the pilgrimage or enter Hajj areas require vaccination against meningococcal disease, polio, and yellow fever. Recommended vaccinations include influenza and COVID-19, the latter of which is required in those who are pregnant, 65 years and older, or have chronic conditions or are immunocompromised. Pilgrims who are elderly or have chronic conditions are also encouraged to ensure they have up-to-date immunizations against additional vaccine-preventable diseases, including diphtheria, tetanus, pertussis, measles, varicella, and mumps.
The nation has implemented enhanced disease surveillance and early detection with the Hajj Health Information System (HHIS) for real-time infectious disease monitoring. In addition, health authorities conduct screening at points of entry to check travelers for symptoms and to review health documents for compliance with required health protocols.
Environmental health and sanitation measures, such as food safety inspections and waste management systems, help prevent health hazards during the Hajj. Saudi Arabia has established strong emergency response readiness, beginning as early as hands-on training during a one-month Hajj rotation for medical residents. Health centers and field hospitals are set up along the pilgrimage route, staffed by 30,000 health workers seconded for the event. Visual triage systems have also been integrated to rapidly identify illness and provide care to patients.
Awareness campaigns are also essential in ensuring the health and safety of pilgrims. Education related to hygiene and respiratory infection measures, such as wearing masks and handwashing, serves as an opportunity to engage and empower the community. Other individual-level protective measures, such as applying insect repellant and wearing protective clothing, can help mitigate vector-borne infections like dengue, malaria, and Zika.
Despite these measures — or perhaps thanks to them — many participants suffer nothing more than a run-of-the-mill respiratory infection, known to pilgrims and health workers as “Hajj cough.” Public health monitoring continues after the Hajj, as the risk of transmission remains present for local and foreign pilgrims, and the communities to which they return.
Managing infectious disease risk at mass gatherings
Conducting health risk assessments, enhancing surveillance systems, and health promotion communication and engagement activities, including immunization recommendations, hygiene rules, and information about where and how to seek medical care are some key considerations for public health authorities in preparing for mass gatherings.
This year’s Hajj is a case of effective public health preparedness that can inform the planning and execution of other mass gathering events. With upcoming international mass gatherings — including the FIFA World Cup in North America, which is anticipated to draw 3 million people, and the Arbaeen pilgrimage in Iraq with an expected attendance of 15-25 million — learning from the successes of other mass gathering events can help reduce the risk of infectious disease outbreaks both locally and globally.
“Infectious disease risk is dynamic. Pathogens we’ve historically controlled like measles and pertussis are reemerging, while new challenges like the recent COVID-19 variant arise,” says Thomas. “So, we need to plan for each mass gathering using a tailored approach informed by robust risk assessments.”
On our radar
- Measles declining in Morocco: The Ministry of Health of Morocco has reported an 80% reduction in measles cases across the country. This substantial decline marks a major public health milestone and is directly tied to a vaccination campaign where over 800,000 doses were administered. The campaign raised the population’s total immunity to over 98%.
- Chikungunya in Sri Lanka: Nearly 17,000 cases have been reported in Sri Lanka to date in 2025, its worst outbreak of the mosquito-borne disease in nearly 20 years. Recent genomic research has identified several unique mutations in the CHIKV virus that may allow it to spread more easily. Nearby nations such as Mauritius, Réunion, India and Pakistan have also experienced a re-emergence of the disease this year.
- Mpox in Sierra Leone: The West African nation is continuing to battle an mpox outbreak, with cases now exceeding 3,000 since the first lab-confirmed case in January. Sierra Leone currently accounts for 75% of Africa’s mpox cases. Rapid case count spikes are being reported in high-density areas, including the capital of Freetown, which has major national and international transit links. The Africa CDC has appealed for more mpox vaccines, and health authorities have announced strengthened measures to protect health workers from infection
To receive global and local outbreak intelligence, sign up here to get every edition of BlueDot’s biweekly newsletter, Outbreak Insider.









