This year’s peak season showed us what we can expect — and what we still can’t predict — for the years ahead
For most of the last century, respiratory diseases were predictably seasonal. Just as you could circle your calendar for hunting season, you could pretty much do the same for flu season: it would peak sometime in late December, wane in early February, and disappear for the rest of the year. Then COVID-19 came along, throwing a wrench into the workings of influenza and its seasonal sidekick, respiratory syncytial virus (otherwise known as RSV). Both the flu and RSV practically skipped an entire season in 2021, only to roar back with a vengeance the following year.
This year’s peak season saw a welcome decline in total activity of influenza-like illnesses (ILIs) compared to last season. But as discussed in the recent BlueDot webinar 2024 Respiratory Trends: Navigating the threat of RSV, Influenza, and COVID-19, that doesn’t mean things are returning to the clockwork predictability of the Before Times. They have certainly not returned to pre-pandemic levels of illness, given the major additional impact of COVID-19.
While there are some clear trends to be found in the most recent data on respiratory illnesses, lots of unpredictability remains. People who work in healthcare-related fields, or who manage medical and health affairs for firms in other sectors, will need to stay on their toes for a while yet. Here is a rundown of what to know — and what to look for.
Respiratory diseases: the trendlines
In the United States, this season’s respiratory illnesses (as measured by percentage of total clinic visits related to influenza-like illnesses, or ILIs) peaked around the last week of December, which is roughly what you’d expect.
Significantly, ILI activity related to diseases such as the flu, RSV and COVID is down more than 4% from last year’s peak. It’s a substantial decline, although as the graph below shows, activity remains well above pre-pandemic levels.
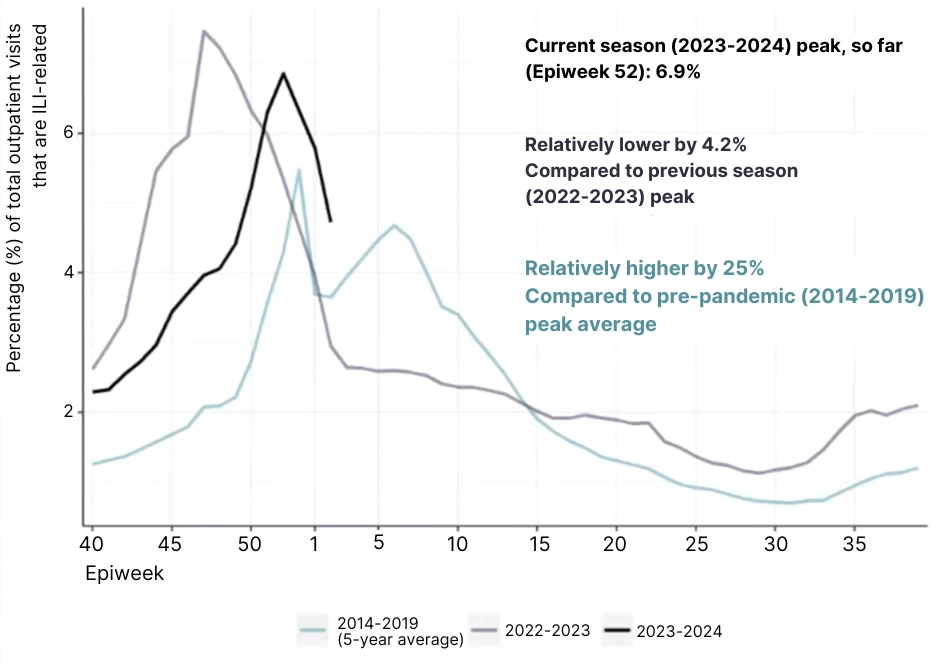
The data might give some readers hope that the trendline could soon close the gap with pre-pandemic averages — in which case they’d be getting ahead of themselves. The graph also shows how today’s ILI season is longer than it used to be: in pre-pandemic times, ILI-related visits would rise above 2% for a period of about 19 weeks, whereas in 2022-23 it was above 2% for 27 weeks, which is more than half the year, and represents a vastly larger total caseload.
What’s more, these trendlines likely undercount the prevalence of COVID-19 cases. Wastewater testing results show that the United States is experiencing its highest levels of SARS-CoV-2 since the Omicron wave of 2022.
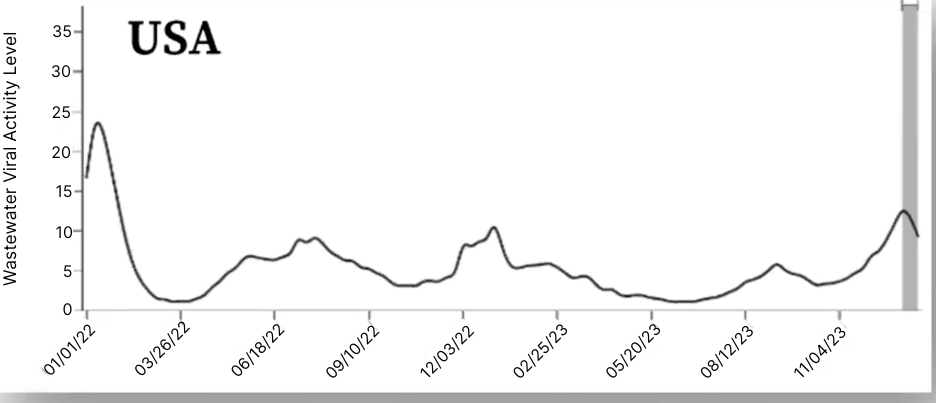
According to BlueDot Senior Epidemiologist Anindita Marwah, “what these high levels could mean is that there may be a large number of people getting infected in the community, but not all of them are seeking health care, not getting tested, and not being reflected in official case counts.”
5 Top Takeaways on
Respiratory Disease Trends
1. Things are definitely not back to normal. Total combined cases of flu, RSV, and COVID-19 are lower than last year. But they are still well above pre-pandemic levels, where they are likely to stay for the foreseeable future.
2. Respiratory illness season lasts longer now. Influenza season starts earlier and ends later than it used to. The same goes for RSV. And COVID is persistent year-round, with multiple peaks throughout the year.
3. Hospitalizations are high, and hospitals are stretched. At this year’s peak, hospitalizations for respiratory diseases were double their pre-pandemic levels. Rates are highest at opposite ends of the demographic scale (under age 5 and over age 65).
4. COVID is still a wildcard. The virus is still mutating, and there’s no guarantee it will trend towards lower severity of disease. COVID testing and reporting is on the wane, making its progress harder to track. And it’s increasingly associated with other diseases, from diabetes to heart disease and cognitive issues. Long COVID remains a serious threat with each infection.
5. Vaccines can help – if people get vaccinated! New RSV vaccines have proven effective but need better rollout to increase uptake. The latest COVID vaccines also target recent variants, yet vaccination rates for the updated vaccines are surprisingly low.
Hospitals and the “seasonal surge”
Even if total disease activity doesn’t accurately reflect COVID’s prevalence, hospitals are certainly noticing its impact. Hospitalizations for respiratory disease, while down 33% from the previous year’s peak, are still double their pre-pandemic levels. “We are seeing dramatically higher rates of total hospitalizations for COVID-19, followed by RSV and then influenza,” says Josephine De Leon, Enablement Specialist in Epidemiology with BlueDot.
Demographically, this season is a continuation of the trend that is showing the oldest and youngest members of society bearing a disproportionate share of total hospitalizations. A majority of hospital stays for respiratory diseases are within the 0-4 and 65+ age groups. And all of this is happening at a time when, in countries around the world, healthcare and hospital resources are stretched thin.
COVID-19: The respiratory disease wildcard
These overall trends, while concerning, are nonetheless showing a generally positive trend: still higher than pre-pandemic levels, but lower than recent seasonal peaks. But it is still difficult to predict that the downward trend will continue, and COVID-19 is to blame for that.
This year’s seasonal peak coincided with the rise of a new COVID-19 variant known as JN.1, which became the dominant strain in December 2023, and by the end of January accounted for 96% of all new infections. The WHO noted that JN.1 is proving highly transmissible, though it does not appear to be causing more severe disease than previous strains.
Unfortunately, there’s no guarantee that future variants will behave the same way. “Viral evolutionary science does not support this notion that disease severity will decrease over time with a virus,” says Marwah. “Severity largely remains a random process that we can’t really predict.”
The world is unlikely to see the kind of hospitalization surge that it experienced with the Omicron variant in 2022 — but there is always the possibility that a new variant will stall, or even reverse, the downward trend of the past year. It’s important to keep in mind that while COVID-19 is a major contributor to the seasonal peak, it has also become a year-round phenomenon all its own, with multiple surges within any 12-month period.
How to beat respiratory disease: vaccines and ventilation
The first line of defense against respiratory disease is population immunity, based upon prior exposure to the disease as well as vaccination rates, both of which protect patients from the onset of severe disease. The good news here is that current vaccines for all three respiratory diseases are effective against currently circulating strains. The bad news is that vaccination rates are fairly dismal.
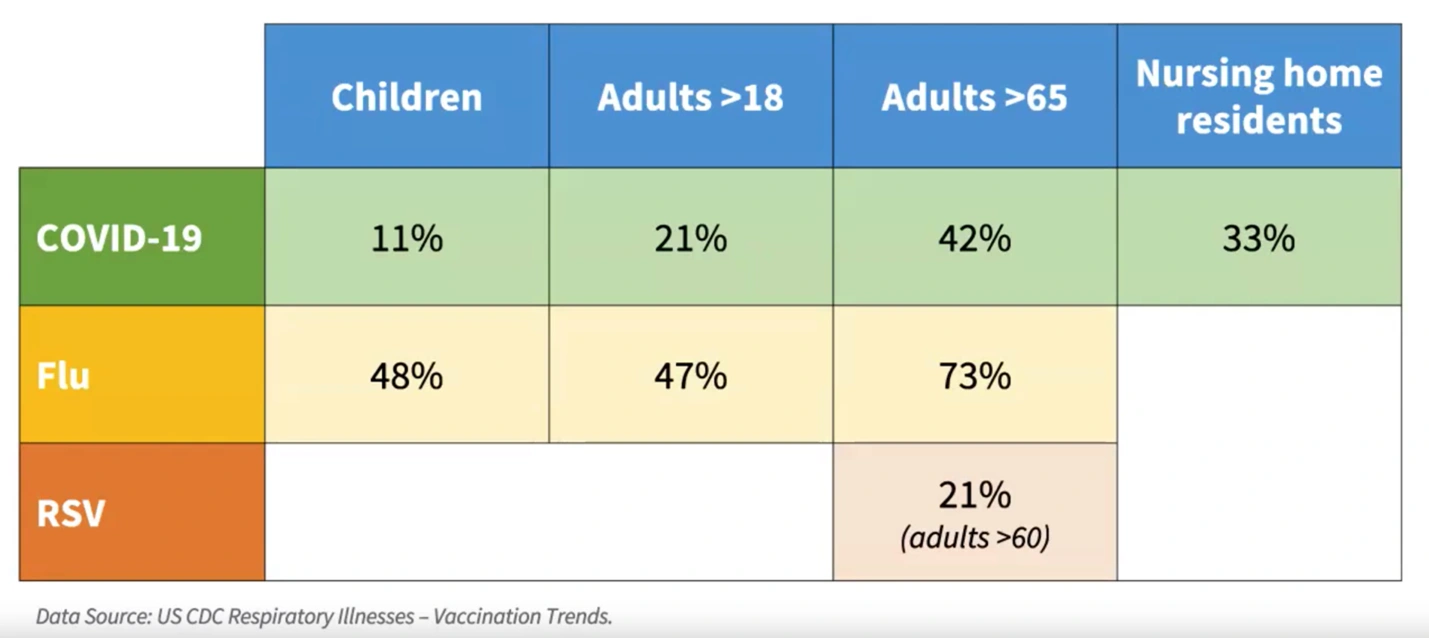
In fairness, current influenza vaccination rates are roughly in line with previous years, while the RSV vaccines for adults over 60, which were only recently developed, didn’t have sufficient runway to be rolled out more broadly within its target population.
However, COVID-19 vaccination rates are surprisingly low for all age groups, including for children and at-risk adults, who happen to be experiencing the highest number of hospitalizations. “There is a lot of work to be done on educating the public about the importance of receiving an updated vaccine for COVID-19 if eligible, especially among children,” says BlueDot Head of Epidemiology Andrea Thomas.
Vaccines likely hold the greatest potential to keep respiratory diseases in check. In addition to COVID-19 boosters and new RSV vaccines, new pharmacological interventions such as mucosal vaccines that prevent infection and pan-coronavirus vaccines may also prove helpful — provided uptake is strong.
Beyond vaccines, there is another measure that any organization can take to help prevent infection if they haven’t already: upgrade its ventilation systems. Advances in ventilation and air filtration have proven effective in protecting staff and visitors from the spread of respiratory diseases. “Here in Toronto, where we are located, the ventilation standards were upgraded for our hospitals following the original SARS outbreak in 2003,” explains Thomas. “So we actually have very good ventilation in our hospitals as a result. But we’re not seeing that yet across the North American hospital sector or in other workplace environments.”