The Northern Hemisphere’s flu season lurks around the corner. Better tracking, surveillance and analysis can help public health officials predict, plan and prevent.
Every fall and winter, influenza-like illnesses (ILIs) — including seasonal flu, respiratory syncytial virus (RSV) and the less predictable COVID-19 — sweep the globe, driving widespread epidemics. Despite their anticipated occurrence, these illnesses are often underestimated as significant public health threats: they are the single largest source of infectious disease hospitalizations annually, applying significant pressures on health care costs and delivery.
The reality is staggering: annually, one billion cases of seasonal influenza alone are estimated worldwide. For up to five million people, influenza infection becomes severe, and tragically, up to 650,000 lives are lost each year. And reported cases are just the tip of the iceberg. Because ILIs are so common and most people show only mild symptoms, many do not access care — which is where cases are tracked. Whether cases are recorded or not, the total economic impact of ILIs is extensive, whether it be productivity loss from calling in sick or hospitalization with severe illness.
“ILIs are one of the biggest problems in infectious diseases globally,” says Dr. Mariana Torres Portillo, Head of Surveillance at BlueDot. “The ability to determine when they may emerge and predicting how big outbreaks might be is fundamental to fortifying our public health response.”
This edition of Outbreak Insider explores global trends in ILIs, including what to expect for the upcoming ILI season in the Northern Hemisphere, and how BlueDot’s cutting-edge tracking methodology and expertise can help.
How the COVID-19 pandemic makes ILI season less predictable
Influenza-like illnesses are a set of respiratory illnesses with overlapping symptoms including fever, cough, and sore throat, with influenza, respiratory syncytial virus (RSV), and COVID-19 being the most impactful in terms of severity and hospitalizations. Transmitted through air and direct or indirect exposure to an infected person or environment, these infections can vary in symptom onset, when and for how long an infected individual may be contagious, severity, and the most appropriate treatment.
Typically, ILIs have a seasonality, with the “flu season” occurring in the fall and winter. In the Northern Hemisphere, this is from October to May, while the Southern Hemisphere’s runs from April to September. Low temperature and humidity, along with movement indoors and reduced immunity, create the ideal environment for respiratory infections to circulate.
The typical seasonality of ILIs shifted in the wake of the COVID-19 pandemic, adding an element of unpredictability that has lasted for years. The US and Australia saw their 2022-23 flu season begin upwards of two months earlier compared with the 2017-2018 season. More recent data, however, suggests that ILI trends appear to be normalizing.
Using real-time event-based surveillance (EBS) and indicator-based surveillance (IBS), BlueDot’s proprietary tracking system is showing that the Southern Hemisphere is beginning to come out of their ILI season, with influenza cases decreasing. Several countries, including Chile, Argentina, and Uruguay, are still experiencing high RSV activity. The flu and RSV tend to circulate together and peak around a similar time. Compared to last year, this year’s peaks did not substantially differ in timing.
Southern Hemisphere influenza and RSV activity, 2024-2025
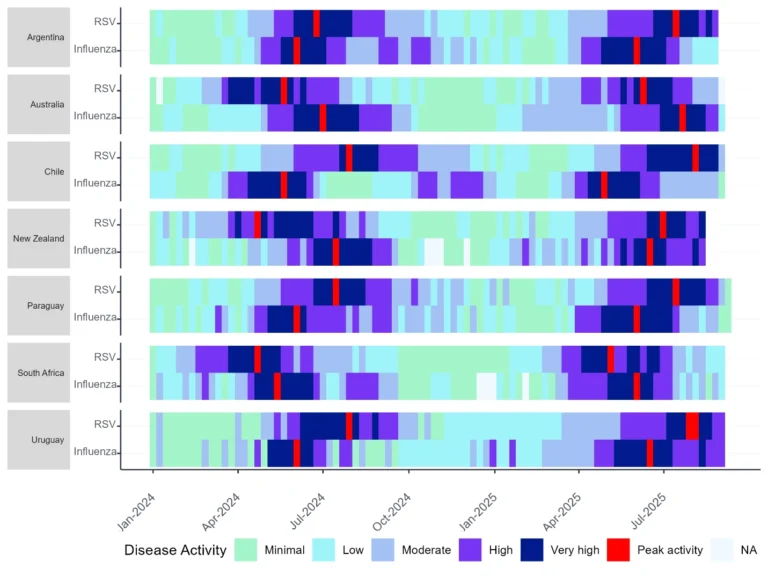
Source: BlueDot, September 14, 2025.
The total volume of cases varied from country to country. Compared to last year, Paraguay reported a 31.8% higher volume of influenza cases nationally, while Chile reported a 31.5% higher volume of RSV cases indicating a more intense season. Uruguay and Argentina, however, had lower RSV case magnitudes than previous years, while New Zealand is still seeing widespread respiratory virus activity, highlighting the still somewhat unpredictable nature of the flu and RSV.
COVID-19 is behaving differently. It tends to hover year-round and does not follow a highly predictable seasonality like other respiratory infections that have been around for much longer in the human population. The spread of new variants of SARS-CoV-2 (the virus that causes COVID-19) through populations with different levels of immunity to past variants still makes it harder to predict year-round, creating challenges for planning, monitoring, and updating vaccines.
Globally, COVID-19 cases have steadily increased, coinciding with ILI season peaks in the Southern Hemisphere. Among countries with available data, almost two-thirds reported an increase in COVID-19 activity in August compared to July, most of which are in the Americas (North and South), Europe, and Japan, indicating a new wave.
Growth rate ratio of COVID-19 case rate, July 28-Aug 24 vs. June 30-July 27, 2025
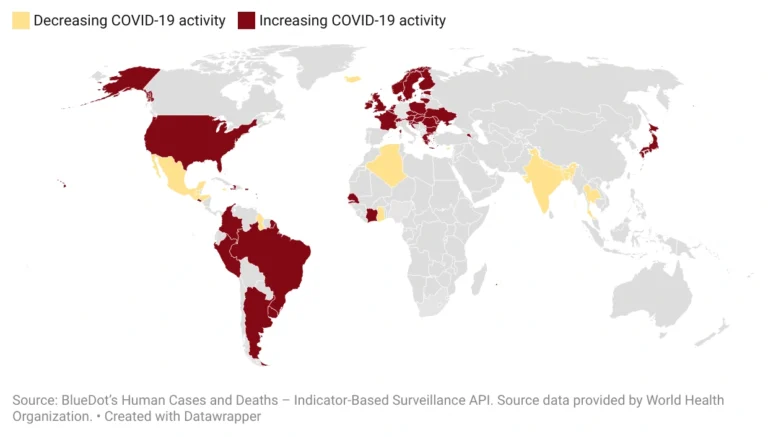
Source: BlueDot, August 24, 2025.
With new COVID-19 waves, new variants emerged. In Asia and Oceania, variant NB.1.8.1 spread quickly, while variant XFG began increasing in Europe and North America. Both have shown signs of evading immune system detection and elimination, while XFG is more dominant globally and increasing in prevalence. With the new school year underway in the northern hemisphere, the risk of further disease spread is expected to increase.
Impact of ILIs
Influenza-like illnesses result in a significant number of hospitalizations and deaths. Young children, older adults, individuals with weakened immune systems or disabilities, and people who are pregnant are at increased risk for more severe illness. Beyond the humanistic burden, seasonal ILIs result in immense healthcare resource use and associated costs. A 2024 US-based study showed that the median length of stay for influenza-related hospitalizations was 3-4 days, and the average cost per influenza-related hospitalization ranged from $11,384 to $14,494.
And when COVID-19 is thrown into the mix, the burden can stress the system beyond normal capacity. Tripledemic pressure, caused by the co-circulation of influenza, RSV, and COVID-19, strained healthcare systems in Latin America. In Chile, for example, pediatric and adult intensive-care unit occupancy rose sharply amid increased respiratory illnesses in late April.
The economic impact is high even among those who do not become severely ill. Indirect costs, such as those resulting from productivity loss, comprise nearly 90% of the flu’s economic burden. Up to 5 days of work are lost due to ILIs, and up to three-quarters of employees miss work for their own or a household member’s illness (called “absenteeism”). Many others continue working while sick (called “presenteeism”), contributing to spread in the workplace. Productivity loss is greater among those who are unvaccinated.
3 Top Takeaways
- Trends in ILIs are starting to normalize. As the Southern Hemisphere comes out of its regular ILI season, influenza and RSV appear to be returning to pre-pandemic levels. Peaks are occurring at similar times, and national cases are generally of similar or lower volume.
- COVID-19 is the ILI wild card. Unlike the flu and RSV, COVID circulates year-round. And its emergence when the flu and RSV are peaking can overwhelm healthcare systems. Variant dynamics are critical in tracking transmission, updating vaccines, and mounting a coordinated public health response.
- ILIs create an enormous economic burden. From missing work (absenteeism) to more severe illness requiring hospitalization, ILIs cause substantial morbidity and subsequent economic impact every year. Public health measures are key in mitigating the effects of these infections on the healthcare system.
Given the immense burden of ILIs on health and the economy, strengthening public health and healthcare system preparation is paramount. Unsurprisingly, vaccination is the gold standard tool for reducing infection and its associated burden. In a recently published modeling study, a universal COVID-19 vaccination recommendation for 2025-2026 was predicted to prevent over 100,000 hospitalizations and 9,000 deaths across the US if there was similar vaccine uptake as observed in 2023-2024. A recommendation limited to only those over 65 years or immunocompromised, in comparison, would be expected to avert 28,000 fewer hospitalizations and 2,000 fewer deaths. (All scenarios assume 2023-24 vaccine uptake levels.) But ongoing vaccine hesitancy, confusion about the benefits of updated vaccination, and varying policies and access to preventatives present a challenge to preparedness, meaning it’s going to be important to know when and how big the inevitable waves may be.
Keeping an eye on ILIs
What do the recent Southern Hemisphere trends mean for the Northern Hemisphere’s upcoming flu season? Often, public health and healthcare professionals can look at trends from the most recent season in the opposite hemisphere in anticipation of what may emerge. Were there new variants of SARS-CoV-2, and what impact did they have? Was this year’s flu season particularly severe? Though these trends may not be the same across hemispheres due to factors such as population immunity and demographics, vaccine policies and uptake, and the ongoing evolution of the pathogens, it does help as a starting point in getting prepared.
Knowing when and how ILIs are circulating impacts crucial decisions that entail millions of dollars, including development and distribution of vaccines and antiviral medications, as well as hospital resource allocation. Closely monitoring ILIs may even detect impending pandemics. In fact, it was BlueDot’s tracking system that first identified and raised the alarms about COVID-19 — even before the WHO and the US Centers for Disease Control and Prevention (CDC).
See ILI Trends in Near Real Time
BlueDot offers a unified view of ILI activity to its clients, offering immediate access to ILI data. BlueDot captures and analyzes official sources, media reports, and wastewater data — all offered to clients on an always-on basis. Our endpoints automatically calculate key insights like incidence, trends, comparison to previous time periods, and other key transformations. Such insights can be easily pulled into internal systems, models and reports. Contact BlueDot to stay on top of what’s happening and what’s relevant to your organization.
“Many of BlueDot’s clients receive global ILI reports, which can be tailored to their geography,” says Torres Portillo. “Receiving both local and global trends every other week based on our surveillance data, or even real-time data feeds, gives them a head start in initiating action.” With infectious diseases, time is of the essence. And with a little more of it, the substantial toll on human health and economic consequences can be improved.
On our radar
- Hand, foot, and mouth disease in Thailand: More than 48,000 cases of HFMD have been reported since the start of the year, marking a nearly 66% increase in cases compared to the same period last year. Cases have been linked to heavy rainfall and high humidity, which create an ideal environment for disease transmission. Despite being endemic, the surge of HFMD exceeds historical averages in magnitude, and the potential for complications highlights the importance of surveillance.
- Leptospirosis in the US: On September 10, an alert was issued following the emergence of an unusual cluster of six cases in northwest Chicago. Up from the historical median of two cases yearly, the increase in this zoonotic bacterial disease has been linked to rodent exposure, highlighting the importance of rodent control in urban settings. Public health efforts are underway, especially for at-risk groups.
- Plague in Mongolia: On September 3, one case of the plague was confirmed in Khövsgöl Province, where the disease is endemic. Six days later, a total of three cases and one death had been reported — exceeding the yearly average. This zoonotic bacterial disease can present in the form of the bubonic, pneumonic, or septicemic plague, and it spreads via contact with infected fleas or rodents. Authorities have strengthened surveillance and enforced temporary lockdowns and closures.
Need to keep up to date on emerging infectious disease outbreaks? BlueDot’s Event Alerts provide the lowdown on outbreaks around the world, delivered to your inbox and tailored to your location and your preferences. Contact BlueDot to stay on top of what’s happening and what’s relevant to your organization.
As ILIs wane in the Southern Hemisphere and pick up speed in the Northern Hemisphere, tracking cases, identifying trends, and anticipating risk is paramount to ensure public health and healthcare systems are equipped to handle outbreaks. BlueDot’s indicator- and event-based surveillance combines data from multiple sources — including wastewater data from across the United States — and can provide details at the regional level, offering a measure of customization for its clients’ priority locations. Combined with ILI Pulse reports offering expert insights, public health practitioners and healthcare professionals can access a tailored view of worldwide infectious disease activity trends.
To stay updated on all the latest infectious disease news, sign up here to receive every edition of BlueDot’s newsletter, Outbreak Insider.









