The biggest summer wave of COVID-19, combined with the annual reemergence of influenza and RSV, pose a considerable burden for businesses
The United States is currently in the midst of the largest summer wave of COVID-19 since 2022, according to wastewater surveillance. Although fewer hospitals are reporting, since June, analyses of case data, test results, and hospital data show surges across the US. COVID-19 levels in wastewater also indicate very high viral activity. The percentage of positive COVID-19 tests reached 17.8%, indicating a high level of community transmission.
Even with fewer hospitals reporting since the emergency stage of the pandemic, COVID-19-associated hospitalization rates are still concerning, especially at a time of year when respiratory disease hospitalizations used to be rare. Similar trends are unfolding around the globe, as nearly 250,000 cases were reported in the last month, up nearly 30,000 cases from a month earlier.
COVID-19 Disease Activity in the US, as of Sept. 7, 2024
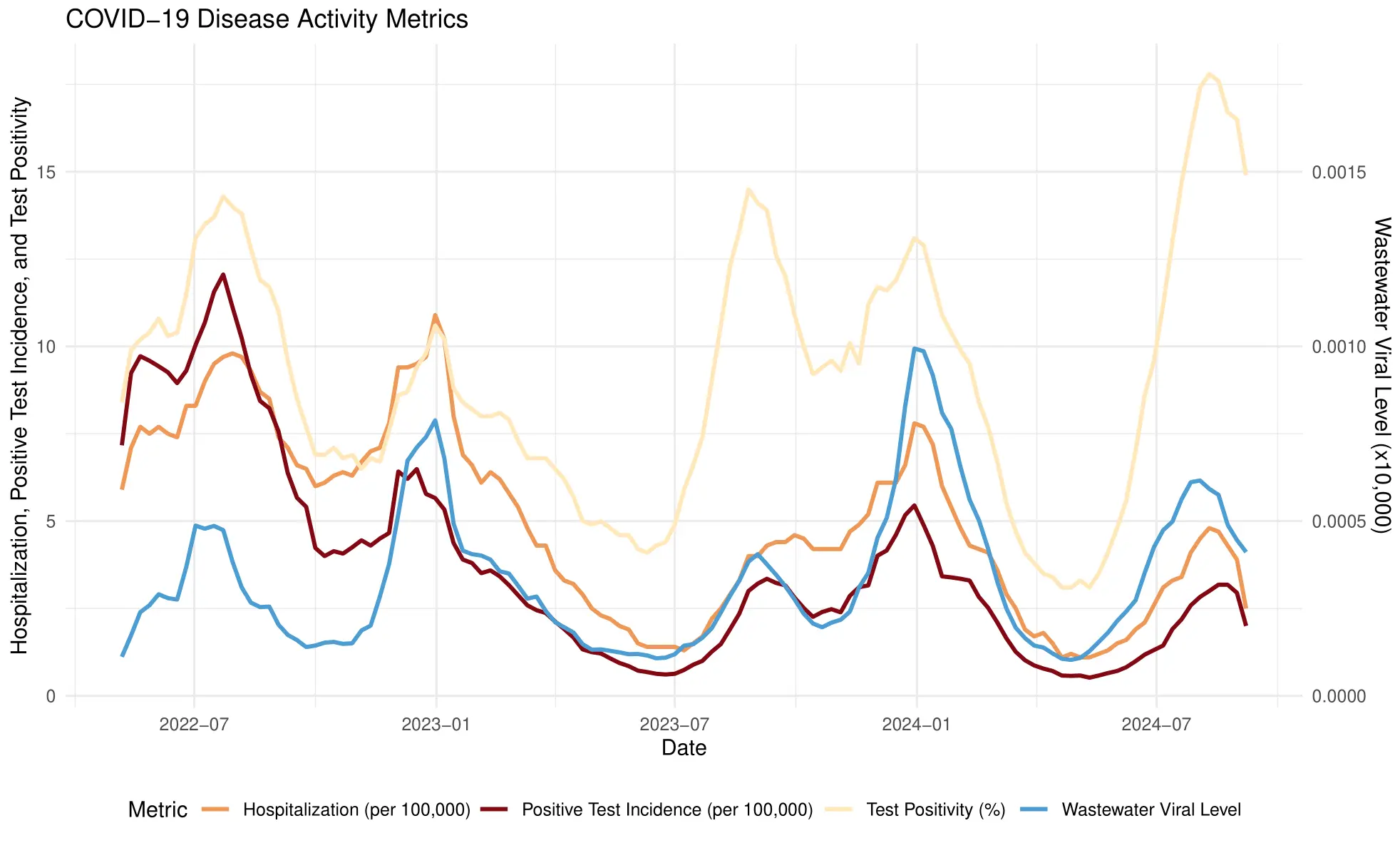
Data sources:
Wastewater Data: BlueDot’s ILI Insights – Wastewater Surveillance API
Test Positivity and Positive Test Incidence Data: BlueDot’s ILI Insights – Indicator-Based Surveillance API
Hospitalization Data: RSV-NET: Respiratory Syncytial Virus Hospitalization Surveillance Network, US CDC
COVID-19 Wastewater Viral Activity Across the US, Sept. 1-7, 2024
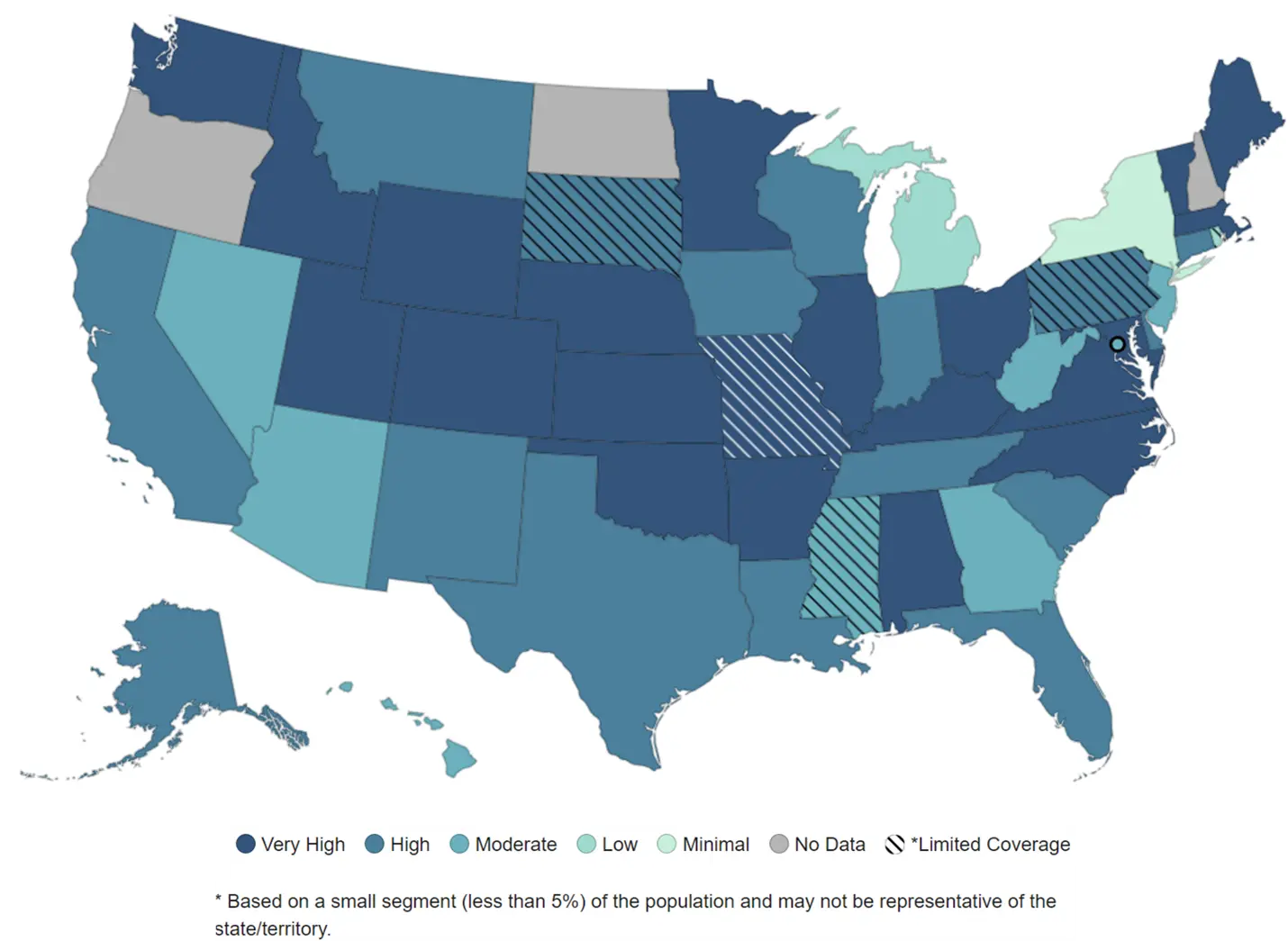
Source: US CDC
According to data compiled by the US Centers for Disease Control and Prevention, overall activity of influenza-like illnesses (ILIs) is 2.5% higher than last year and 109% higher than the five-year pre-pandemic average for the same epiweek. The data reflects both a significant year-over-year increase and the “new normal” of the COVID era.
And we are just at the outset of respiratory disease season, when other viruses are soon sure to circulate. Given the anticipated fall and winter contribution of seasonal viruses like influenza and RSV, experts are concerned about the compounding effect of these viruses on the healthcare system and the economy.
“These next few weeks are pivotal,” says BlueDot data scientist Lauren McKenzie. “We’re at a fork in the road as seasonal respiratory illnesses surface.” While this issue of Outbreak Insider focuses on data from the United States, the situation is global in scale. Business leaders around the world would be wise to prepare for the prospect of increased absenteeism due to illness in the months ahead — and, more importantly, take steps to prevent it.
A rundown on respiratory infectious diseases
Respiratory diseases, such as COVID-19, influenza, and RSV, are caused by viruses that affect the upper and lower respiratory tract. These viruses each spread through a unique combination of airborne transmission and direct or indirect exposure to an infected person or environment. SARS-CoV-2 predominantly spreads through the air, for instance, while the relative contribution of other modes of transmission may be somewhat different for flu and RSV.
Commonly described as influenza-like illnesses (or ILIs), symptoms of these respiratory infections typically include fever, chills, cough, and sore throat. Given that these illnesses are caused by different viruses, they vary in the time to symptom onset, the severity and persistence of symptoms, when and for how long an infected individual can spread the virus, and the most appropriate treatment. Respiratory infections can be mild to severe in nature, and they result in a significant number of hospitalizations and deaths. Young children, older adults, individuals with weakened immune systems or disabilities, and people who are pregnant are at increased risk for more severe illness. A growing body of evidence also documents the long-term effects that can result from these infections, especially SARS-CoV-2, even in previously healthy individuals.
Cases of COVID-19 began rising in June, which is earlier than observed in previous years as a result of new variants of the SARS-CoV-2 virus and waning population immunity. Unlike other respiratory illnesses, COVID-19 does not follow dependable seasonal patterns because it is continuing to evolve so rapidly. Meanwhile, seasonal ILIs such as seasonal flu and RSV are expected to rise in the weeks ahead. While signs of activity for these viruses remain low for now, the return to school will impact disease transmission — a trend already being observed in emergency department visit data.
US National Viral Levels Across Respiratory Illnesses, as of Sept. 14, 2024
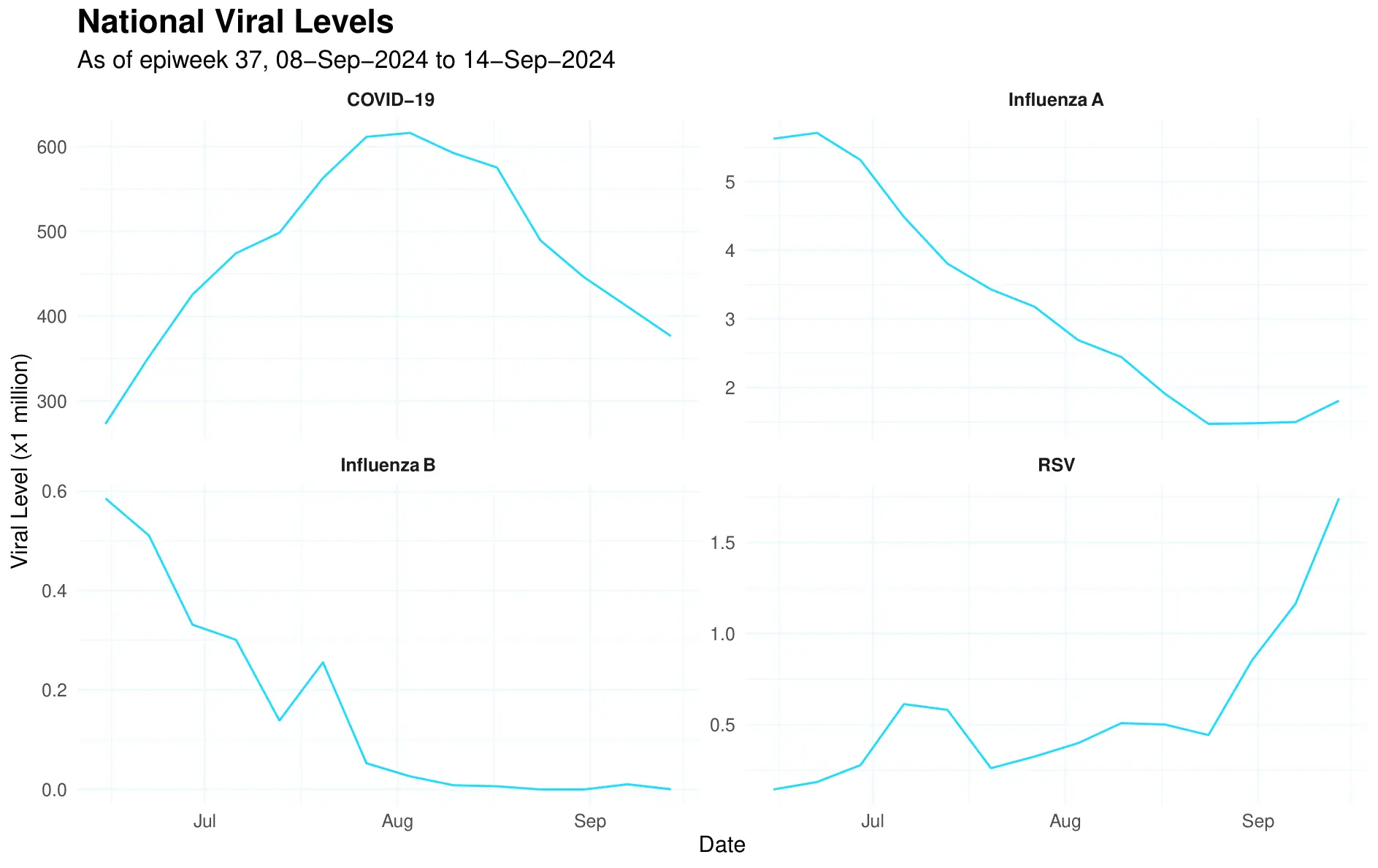
Source: BlueDot’s ILI Insights — Wastewater Surveillance API
Note: The viral level categorization indicator will also be available through this endpoint in upcoming months.
The impact on health systems — and on businesses
With flu season around the corner, the co-circulation of respiratory viruses, including SARS-CoV-2 (the virus that causes COVID-19), influenza, and RSV poses considerable pressure on the healthcare system. For instance, the 2023-2024 season saw a COVID-19-associated hospitalization rate of 183.7 per 100,000 people in the US. Compared to the seasonal flu, the risk of death from COVID-19 was found to be 60% higher. While the impact of COVID-19 has dramatically lessened from the height of the pandemic, more than 1,000 people have been dying from it weekly this summer in the US. Additionally, the 2022-2023 US flu burden amounted to an estimated 31 million cases, 360,000 hospitalizations, and 21,000 deaths. Annual hospitalizations for RSV in the US are also concerning, with up to 80,000 hospitalizations among children under 5 and 160,000 among adults 60 or older.
Consequently, respiratory illnesses have a profound societal and economic burden, and no organization is immune to their impact. Up to 75% of employees miss work due to their own infection with ILIs or because of infection among household members. More specifically, the first two years of the COVID-19 pandemic saw an estimated 6.6 billion work hours lost, resulting in $213 billion in costs to employers. A substantial economic burden was also reported for the flu and RSV in the US. The annual economic burden of seasonal influenza was estimated at $11.2 billion, $8 billion of which is attributable to indirect costs such as productivity loss (absenteeism and presenteeism). Recent evidence of US adults aged 60 years or more found that RSV had an annual economic burden of $6.6 billion. Of this, $2.9 billion was attributed to direct medical costs and $1.1 billion was attributed to indirect costs due to productivity loss. Together, viral respiratory infections have a major impact on businesses and organizations of all kinds.
Top Takeaways
- COVID-19 cases surge in the largest summer wave since 2022. Reported case counts and viral wastewater levels show substantial COVID-19 activity in the US — and globally.
- Simultaneous respiratory viruses raise risks for both healthcare systems and businesses. As back-to-school season spurs the start of flu season, the uncertainty of COVID-19’s trajectory combined with seasonal influenza and RSV present considerable societal and economic burden.
- Preventing productivity loss with public health measures. To mitigate the risk of viral respiratory illness on workplaces, vaccination, improved ventilation, and clear workplace policies are pivotal.
Reducing the risk of respiratory illnesses
As with other infectious diseases, the best prevention against severe illness from SARS-CoV-2, influenza, and RSV is vaccination. Yet vaccination rates are low. Only about 43% of Americans have gotten or plan to get the updated COVID-19 vaccine and a slightly higher proportion — 56% — plan to get the flu shot. Effective RSV vaccines are now available to high-risk populations which, if optimally delivered, could have a major impact on the burden of this disease. Workplaces can promote vaccination by providing education and removing barriers to accessing vaccines, such as encouraging employees to get immunized during work hours. While current vaccines are imperfect at preventing the spread, the research shows that getting an updated COVID-19 vaccine is linked to having a lower amount of virus in our upper airways, as well as reducing the risks of severe illness and Long COVID. This means that greater vaccination coverage with recent vaccinations can lead to greater community immunity, so it’s harder for the virus to spread. This is especially important for the health and safety of those who cannot get vaccinated.
Employers can also consider revisiting their infection control measures. For example, providing access to personal protective equipment, such as respirator-style masks, at-home tests and hand sanitizer, can encourage their use to help reduce the spread of viruses at work and in the community. Workplaces can also assess their ventilation, making improvements to reduce respiratory pathogens in the air and adding air cleaning where needed. This is especially important in densely populated indoor settings that serve as major drivers of respiratory infectious disease spread, such as offices, schools, and hospitals. Better air quality, combined with mask-wearing, has been shown to reduce SARS-CoV-2 transmission by 90%, which can mitigate productivity loss. This is a benefit increasingly realized by organizations around the globe, such as Amazon, which invested in improved air quality systems to prevent the spread of infectious diseases. Not only would measures to reduce transmission of SARS-CoV-2, seasonal flu and other respiratory viruses benefit us now, but they would mitigate against the threat of future respiratory pandemics. With the continued circulation of H5N1 influenza in dairy cows across the US, and the concern about the co-circulation of human influenza this winter, mitigating against a future respiratory pandemic feels ever-more urgent.
Organizations can also reduce the risk of workplace respiratory illness by developing or enhancing their workplace policies. For one, workplaces can encourage sick employees to stay home until they are no longer contagious and promote mask-wearing if this is not always feasible. Flexible leave and remote work policies are important incentives to ensure sick employees do not spread infection at work. Finally, employers can consider adopting or expanding paid sick leave programs — an investment that has shown significant cost savings to employers. Paid sick days are also beneficial to an already overwhelmed healthcare system. According to the National Partnership for Women & Families, with paid sick days, the US would prevent 1.3 million emergency department visits and save more than $1 billion per year.
“We know there are major healthcare constraints globally, not to mention the risk to healthcare workers,” says Andrea Thomas, PhD, BlueDot’s Head of Epidemiology. “We have the knowledge, aerosol expertise and technologies to substantially tackle this problem. We are not back in 2019 anymore because we continue to confront the added burden of COVID-19. We can adapt to this new world by applying the improved knowledge we have about how these viruses spread, mitigating the negative effects of ILIs on businesses and society at large.”
BlueDot is at the forefront of monitoring infectious disease trends and outbreaks around the globe. The ILI Pulse reports, published bi-weekly, incorporate hospital data, case data, testing data, virus strain and variant data, and wastewater surveillance to offer a holistic view of infectious diseases circulating regionally, nationally, and globally. As we head into flu season, stay on top of respiratory viruses by subscribing to our Pulse reports. Get in touch to learn more.









