Once largely confined to Africa, the disease has taken hold in all parts of the world — with consequences for travelers and public health alike
The spread of chikungunya, the mosquito-borne disease that causes debilitating joint pain, has resulted in more than 270,000 cases and 110 deaths to date in 2025 across southeast Asia, Europe and the Americas. As cases continue to rise, the World Health Organization has issued an alert for a potential global chikungunya epidemic — a surprising turn of events for a disease usually considered regional in nature.
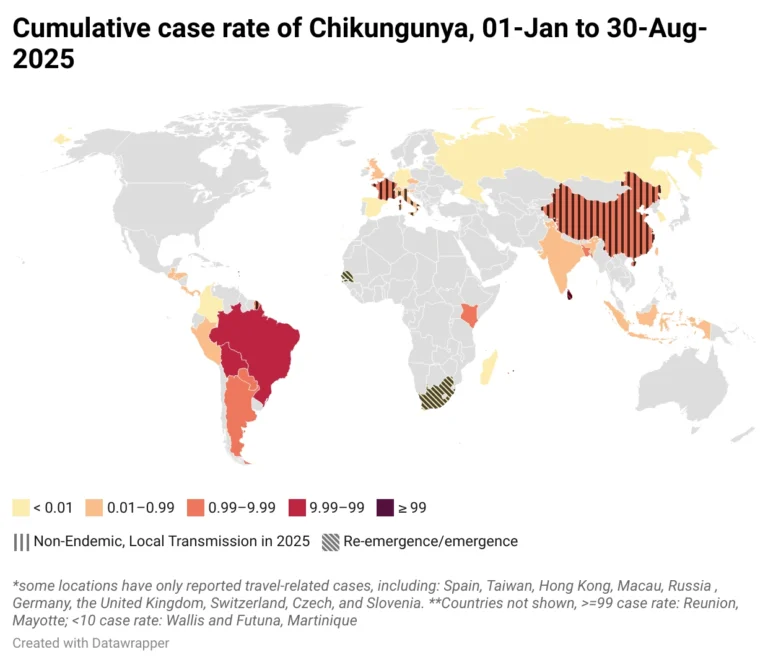
As of mid-August, about 120 countries are affected and more than five billion people are at risk. Cases have been both imported and locally-acquired in new locations, highlighting the risk of global travel and the growing concern of increased vector suitability and expanded habitats as the climate changes. For public health officials, that can mean increasing their surveillance for imported cases, educating local medical professionals on the likelihood of local cases, and even implementing vector control measures.
“Chikungunya is a major public health risk that is expected to keep spreading to new locations,” says Andrea Thomas, PhD, BlueDot’s Head of Epidemiology. “The key to prevention is knowing where it’s most likely to emerge next.”
This edition of Outbreak Insider dives into where chikungunya outbreaks are occurring, where risk of infection is heightened, and what public health officials can do to assess the risk level in their region.
Chikungunya: the lowdown on an alarming arbovirus
First discovered in Africa in the early 1950s, chikungunya is a vector-borne disease caused by a virus of the Togaviridae family. The illness is transmitted by the Aedes mosquito, an aggressive species most active during the day. These mosquitoes tend to live in close proximity to humans and thrive in warm and wet conditions across tropical, subtropical, and temperate climates.
The name “chikungunya” is based on the Kimakonde words for “to become contorted,” a reference to its most tell-tale symptom: severe joint pain. For up to 40% of those infected, joint pain is chronic. However, the disease’s often-mild initial presentation, and its overlapping symptoms with other arboviruses like dengue and Zika — fever, headache, rash, fatigue — make it challenging to identify. There are an estimated 35.3 million infections around the world annually, of which barely half (17.7 million) are symptomatic. Chikungunya is estimated to cause 848,000 chronic sequalae, 3,700 deaths, and 121,000 disability-adjusted life years (DALYs) lost every year.
Climate change, increased global travel, urbanization and land use changes, and decline in global surveillance investment are among the key factors responsible for the recent explosion of chikungunya and other mosquito-borne diseases. Climate change is a notable driver of disease as rising temperatures, longer summers, milder winters, and changes in rainfall patterns increase the geographic range in which mosquitoes can thrive.
And where Aedes mosquitoes are present, there’s a high correlation that chikungunya is as well. The virus has now made landfall on most continents. Unlike dengue, which has predicable seasonal patterns, chikungunya is cyclical, rising and falling over multi-year intervals — and when outbreaks occur, they can be sporadic and explosive. Well over half of the world’s countries, largely in Africa, Asia, and the Americas, are reporting cases. And today, the virus is establishing a foothold in Europe.
Source: BlueDot, September 2025.
Chikungunya in 2025: a disease spreads its wings
In the first half of 2025, BlueDot issued alerts for outbreaks in Réunion, Mayotte, and Mauritius, where more than 50,000 cases have been reported since August of last year. India, where the virus is endemic, was the center of an atypical spike in cases last fall with a historical 180,000 laboratory-confirmed cases. And nearby Sri Lanka is also battling widespread cases with unique genetic findings that help the virus spread more easily and evade immune system detection.
Outbreaks in the Indian Ocean region have spread to Africa and Europe, including in France, Russia, and Germany. Travel-related cases have prompted the United Kingdom Health Security Agency and the US Centers for Disease Control and Prevention (CDC) to issue travel warnings and precautions. BlueDot’s air connectivity analysis — which clients use to model the risk of imported cases between travel hubs for any part of the world — found that outbreaks in India had a high risk of spread to the United Arab Emirates, and moderate risk of spread to the UK, US, and Singapore, among others.
3 regions with major chikungunya outbreaks in 2024-25 and their connectivity to North American and European travel hubs

Source: BlueDot, September 2025.
The virus’ introduction to areas with large, immunologically naïve populations means the disease can be transmitted quickly, and fiercely.
China — which experienced a combined total of 519 chikungunya cases from 2010 to 2019 —has reported more than 10,000 cases of chikungunya since July of this year, marking the country’s largest recorded outbreak. At its peak, over 600 new infections were being reported daily. The epicenter is Guangdong, the southeast Chinese province that also happens to be the nation’s most populous.
Despite China’s efforts to clear mosquito breeding grounds, spray insecticide, and establish mosquito-proofing efforts, imported cases have been detected in Taiwan, Macau, and Hong Kong. This has prompted travel advisories to be issued for southern China. BlueDot’s air connectivity also indicates high connectivity risk to Malaysia and Thailand, and moderate connectivity risk to Japan, South Korea, and Cambodia. For some of these countries, an outbreak would strain an already resource-limited healthcare system.
Europe, whose populations are also naïve to chikungunya, has seen a record-breaking 27 outbreaks this year as of August 20, a combination of both local and travel-related transmission. The Alsace region in northeastern France recorded its first-ever locally acquired case this year, meaning transmission risk is expanding northward. The presence of Aedes albopictus, one of the two types of mosquitoes that carry the virus, has now been established in 16 European countries and 369 regions — an increase from 114 regions just ten years ago.
Get real-time coverage of fast-moving diseases
Over the past 18 months, BlueDot has sent over a dozen alerts to our clients on the global spread of vector borne diseases including dengue, chikungunya, zika and malaria. We’ve tracked cases from recently affected areas like Russia, Spain and the United States. Our alerting complements our ongoing, up-to-date case data on these diseases, which syncs official sources and media reports in a single experience.
In the Americas, a suspected 212,029 cases and 110 deaths were reported between January and mid-August. Since the disease arrived on the shores of the Americas in 2013, Brazil has consistently experienced the highest case counts in the world, reporting more than one million cases since 2019. From 2020 to 2024, there has been a 41.5% average year-on-year increase in chikungunya cases.
A 2024 analysis conducted by BlueDot found that global travel advisories for chikungunya in Brazil decreased over time despite an increase in yearly cases. Since travel advisories are typically issued for new outbreaks — not ongoing endemic activity — a gap emerged in travel advisory issuance and actual disease activity. Given Brazil’s high connectivity to North America, public health officials need up-to-date intelligence to reassess their local and regional needs for extra precautions in preventing illness and monitoring imported cases.
3 Top Takeaways
- Global chikungunya cases have become a game of Whack-A-Mole. From Asia to the Americas, record-breaking outbreaks have been reported. This sporadic, unpredictable, and explosive mosquito-borne disease has popped up in expected and unexpected places largely due to global travel and climate change.
- Connection to chikungunya is too close for comfort. Imported and locally acquired cases are emerging in endemic and non-endemic areas, leaving more than 5 billion people at risk of infection. BlueDot’s air and ground connectivity analysis shows the most connected locations in Europe and North America to global outbreaks.
- Mobilizing preventive tools can mitigate mosquito-borne diseases. Predicting risk and establishing connectivity to hotspots can lead to decreased chikungunya infections, thereby reducing the associated disease burden.
Arboviral awareness
Chikungunya presents both public health officials and workplace health and safety directors with a potentially immense patient and economic burden. Between 2011 and 2020, chikungunya’s 18.7 million global cases and resultant 1.95 million DALYs amounted to an estimated $50 billion USD in total economic burden. Of this, $2.8 billion was attributed to direct costs, and $47.1 billion in indirect costs, most notably absenteeism. And a global epidemic of chikungunya in the months ahead would not be its first.
All of which underlines the importance of regional risk assessment for chikungunya. Some interventions, such as physician education and increased vigilance for imported cases, can be implemented through existing local practices. Funding for vector control programs, on the other hand, tends to be cyclical and reactive — meaning that regions newly at risk of local chikungunya transmission could be facing significant budget pressures, increased costs, and response delays.
“BlueDot’s clients in the public health sector are leveraging our surveillance data and predictive tools with other official sources to better serve their populations,” says Thomas. “The intelligence they get as a result is timelier and more comprehensive than traditional approaches.” With the best infectious disease intelligence, public health authorities and healthcare professionals can keep their finger on the pulse and protect countless people from illness.
On our radar
- Ebola in the DRC: In early September, 28 suspected cases and 16 deaths were reported, confirming a new outbreak of Ebola in the Democratic Republic of the Congo. Response teams have been deployed, along with two tonnes of supplies and 2000 doses of the Ervebo vaccine. The genomic evidence, swiftly provided by DRC officials within 24 hours of the outbreak declaration, indicates a new zoonotic spillover event from an unknown reservoir host, underscoring the continuous threat of outbreaks in this region.
- Eastern Equine Encephalitis in Canada: Canada saw its first human case of EEE in Hamilton, Ontario, among a man with no recent travel history, meaning the case was likely locally acquired. Two horses in the area were also confirmed to have the mosquito-borne virus, further indicating local exposure and risk. Although rare, cases in 2024 and 2025 suggest vector habitats have expanded, and exposure to the disease may increase with climate change and lengthened mosquito seasons.
Need to keep up to date on emerging infectious disease outbreaks? BlueDot offers daily reporting, tailored to your location and your preferences, that can be delivered to your inbox or synced to your internal reporting tools. Contact BlueDot to get real-time data on what’s happening and what’s relevant to your organization.
BlueDot’s indicator- and event-based surveillance, regional connectivity analyses, and expert insights into hotspots and areas of increasing risk complement travel advisories and local responses, giving public health experts and healthcare professionals a more holistic view of infectious disease activity.
To stay updated, sign up here to receive every edition of BlueDot’s biweekly newsletter, Outbreak Insider.
Curious to learn how BlueDot saves clients hours per day tracking infectious disease? Click here to connect with us.









