Brazil — the global hotspot for chikungunya — reports yet another outbreak, and becomes the first endemic nation to approve the vaccine
On April 6, a severe chikungunya outbreak was confirmed in Santa Catarina, Brazil. The small Brazilian state southwest of Saõ Paulo has reported 379 lab-confirmed cases and three deaths so far this year — more than eight-fold higher than the same time last year.
The intense local outbreak is part of an ongoing nationwide epidemic, as confirmed cases approach 45,000 in Brazil year-to-date. Like Santa Catarina, which is also reporting an additional 535 probable cases, total cases in the country are likely much higher. The Pan American Health Organization (PAHO) estimates close to 100,000 total cases in 2025 should be expected.
The situation in Brazil is part of a broader global trend for the disease. Last year, there were a total of 627,300 cases and 213 deaths globally, representing a 22% increase compared to 2023. So far this year, approximately 80,000 cases and nearly 50 deaths have been reported worldwide. And as with Brazil, these official case counts surely underestimate the true total.
“The true disease burden and risk of chikungunya is difficult to quantify given challenges with detection and diagnosis,” says Andrea Thomas, PhD, BlueDot’s Head of Epidemiology. New clusters along with over 420,000 cases in Brazil last year — a historic high for the country — reflect the virus’s silent and uncontrolled circulation across the country.
As Brazil ushers in its eleventh consecutive year of chikungunya outbreaks, the risk of international spread within Latin America and beyond continues to grow. And as travelers arrive to endemic areas from around the globe, the need for more effective surveillance and outbreak communication, including vaccine availability, is critical.
A chronology of chikungunya
Chikungunya is a vector-borne infectious disease primarily transmitted by Aedes aegypti and Aedes albopictus mosquitoes. Acutely, chikungunya symptoms are similar to other arboviruses: fever, headaches, and muscle and joint pain. However, it’s the severe joint pain, which is chronic in up to 40% of those affected, that gives the disease its name.
The illness was first identified in Tanzania in 1952 before spreading across the continent; its name comes from the Kimakonde language, meaning “that which bends up.” By the late 1950s, the virus had emerged in Asia, with notable outbreaks Thailand and India. Europe saw its first cases more than 40 years later, with an outbreak in Italy in the mid-2000s. But it wasn’t until 2013 that the disease was reported in the Americas, when an outbreak erupted on the island of Saint Martin.
In the 12 years since, the Americas have become the epicenter of chikungunya outbreaks, with at least 45 countries across the region reporting more than 3.7 million cases. Over time, annual case counts have increased: more than 400,000 cases were reported last year, up from under 200,000 in 2019.
Chikungunya Cases by Subregion in the Americas, 2019-2024
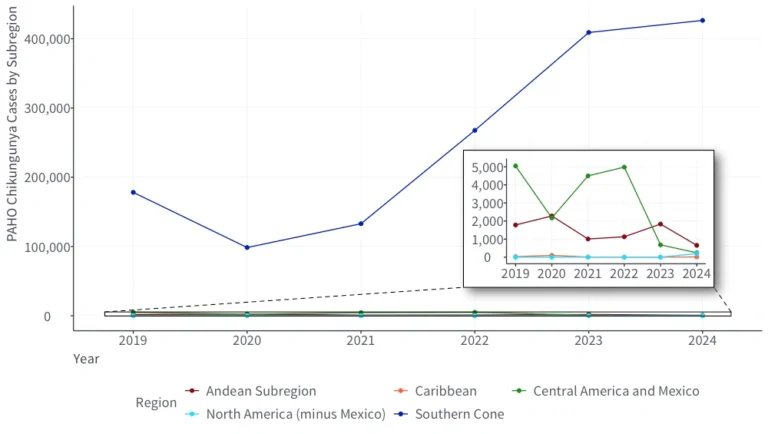
Source: BlueDot, April 17, 2025
Brazil is the hardest hit country in the world; chikungunya outbreaks have persisted for 11 years. Comprising nearly all cases in the Americas region, Brazil reported 420,139 cases and 236 deaths last year. Over one million cases have been recorded since January 2019. And from 2021 to 2024, a 41.5% average annual increase in cases has been observed. Other countries in the Americas also reported unusually high case counts last year, including 3,314 in Paraguay and 1,388 in Argentina.
Despite primarily causing disruption across the Americas, chikungunya has continued to spark outbreaks around the world, with more than 110 countries identifying chikungunya cases to date. Currently, most continents are reporting cases, whether from local or travel-related transmission. Over 190,000 cases were reported last year in India, where the disease is endemic, some with atypical and severe symptoms potentially attributable to viral mutations. Meanwhile, the island of Réunion, near Madagascar, detected its first locally acquired cases in over a decade. Since the start of the year, the island has seen 33,835 cases and six deaths, prompting the director general of the hospital center to call for reinforcements to help with the crisis.
Global Incidence of Chikungunya, January 1, 2024-April 16, 2025
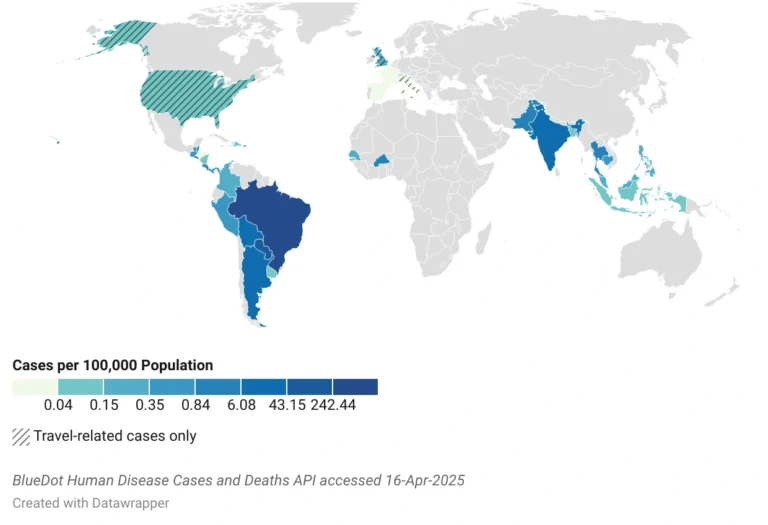
Most cases occur in tropical and subtropical areas with substantial vector presence and a suitable climate. But as is the case with other vector-borne diseases, climate change, expansion of vector habitats, viral adaptation, urbanization, and increased travel lead to greater risk of spread. More than ¾ of the world’s population is estimated to live in areas at risk of the disease, and this number is expected to grow.
Chikungunya communication breakdown
As annual chikungunya cases rise to new heights and the disease emerges or remerges in countries around the globe, clinicians and officials continue to face difficulty detecting and diagnosing the disease. Amid limited lab capacity, mild acute presentation, and overlapping symptoms with other arboviruses, the true burden of disease is not well understood. Consequently, people remain unaware of their risk of exposure.
In a recent analysis conducted by BlueDot to better understand whether official outbreak declarations or travel advisories sufficiently characterized exposure risk, both globally and within Brazil, less than half of global outbreaks reported since 2010 were declared by the WHO, US CDC, or ECDC. National declarations and travel advisories were also lacking for Brazil, despite evidence of the virus’s circulation in different parts of the country occurring at any given time. In fact, chikungunya cases between January 2021 and July 2024 often surpassed expected seasonal baselines.
Global Outbreaks (red) and Official Outbreak Declarations and Travel Advisories (yellow), 2010-2024
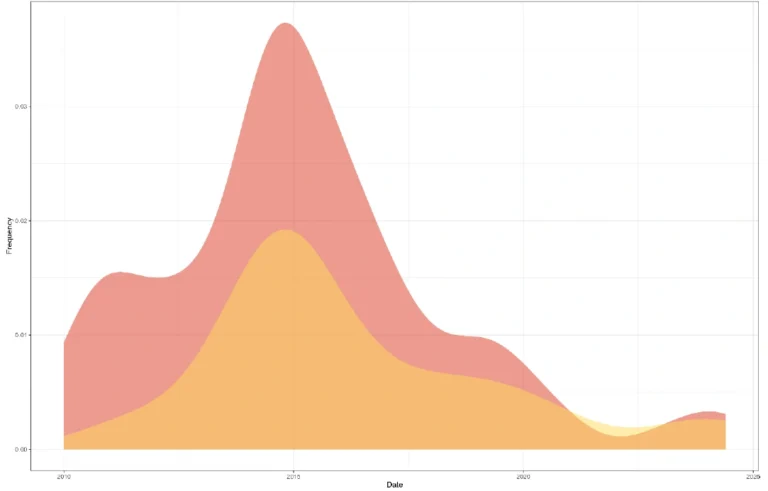
Source: BlueDot Chikungunya Outbreaks Report, Updated September 16, 2024
The analysis concluded that communication around chikungunya cases, especially outbreak declarations and travel advisories, are inconsistent and lack the information needed to protect people from infection. As cases continue to surge at alarming rates among endemic populations and travelers to these regions, bolstered public health efforts are needed to ensure risk is communicated.
3 Top Takeaways
- Chikungunya spreads brazenly across Brazil and the Americas. Brazil has confirmed nearly 45,000 chikungunya cases and 57 deaths in 2025 so far, marking the eleventh consecutive year of outbreaks in the nation. The country comprises most of the cases across the region, tallying more than 3.7 million in the decade since the disease was found there.
- Hindered communication, hidden risk. Outbreak declarations and travel advisories by official organizations have been issued for less than half of identified outbreaks globally since 2010. And as chikungunya often goes undetected and unreported, the true burden is unknown.
- Importance of increased immunization. Brazil recently became the first endemic nation to approve a new chikungunya vaccine. With two approved vaccines so far, immunization against chikungunya is a promising new development for widespread protection and prevention of severe, chronic illness from chikungunya.
Abating the arbovirus
Chikungunya is a major public health concern requiring enhanced disease prevention and control, especially in endemic nations such as Brazil. Strengthening surveillance and diagnosis, tracking and communicating outbreaks, improving disease awareness, continuing vector control practices, and implementing immunization programs are key steps needed to mitigate risk, especially in the absence of antivirals.
On April 14, Brazil became the first endemic country to approve Valneva’s chikungunya vaccine, which had previously been approved in North America, the EU, and the UK. This follows the approval of the second chikungunya vaccine in the US and Europe, developed by Bavarian Nordic. With available vaccines, the next step will be widespread immunization in endemic countries and for travelers to these regions.
It’s estimated that even 50% vaccine coverage with a vaccine that is 70% effective against disease, 40% effective against infection, and offers 5-year protection would result in almost 5 million fewer infections, 651,000 fewer chronic cases, 209,000 disability-adjusted life-years (the number of years lost due to morbidity and mortality), and 3,750 fewer deaths globally per year. Considering the high rate of chronic joint pain and the risk of severe complications, including myocarditis, encephalitis, and Guillain-Barré syndrome, vaccination is expected to mitigate the disease’s associated extensive health and economic consequences.
“The risk of chikungunya is only going to increase,” says Thomas. “As geographic distribution expands and prevalence increases, ensuring vaccines are offered to those most at risk will make a huge difference in controlling outbreaks.”
On our radar
- Measles in the Americas and Asia: On April 13, Belize reported two confirmed cases of measles, marking the country’s first confirmed cases in over 30 years. The week before, Taiwan reached a six-year high with 22 confirmed cases, doubling rates from the same period a year prior. Imported cases are driving counts in both nations as the virus is spreading across these regions, including in Cambodia and Mongolia, where hundreds have been infected. The measles resurgence is posing a global threat, underscoring the importance of vaccination.
- Mpox in Europe: In the last few weeks, Germany, the UK, and Switzerland have detected mpox clade Ib — the latter nation’s first imported case. While primarily among travelers returning from areas where the virus is circulating or those linked to someone who traveled, the source of the UK case is unknown. Imported cases of mpox clade I have previously been reported across other European nations, including Belgium, Ireland, and France as mpox remains a Public Health Emergency of International Concern.
- Yellow fever in Uganda: On the heels of the outbreak that has erupted in South America, yellow fever has emerged in Uganda. Six cases were confirmed, sparking a mass vaccination campaign on April 10. Immunization efforts are aiming to protect 4.3 million people in the country, where the virus is endemic.
To stay informed about outbreaks at home and around the world, sign up here to receive every edition of BlueDot’s biweekly newsletter, Outbreak Insider.









